To the editor:
Donor-related malignancy is a rare complication after solid organ transplantation. We present a unique case of a patient with donor-derived acute myeloid leukemia (AML) after kidney transplantation.
A 69-year-old male presented with fatigue, fever, diarrhea, and vomiting. He had a history of polycystic kidney disease and had received a double deceased kidney transplant from an 81-year-old woman 2 years earlier. The preadmission post-transplant clinical course was uneventful. Current immunosuppression consisted of tacrolimus (3 to 5 mg/day), mycophenolate mofetil (500 mg twice daily) and prednisone (15 mg daily). At presentation, the patient was ill-appearing with aphthous stomatitis and lower limb edema. Laboratory analysis of the peripheral blood revealed pancytopenia without evidence of blasts (supplemental Table 1). Antibiotic treatment (Ceftriaxone) for assumed infectious gastroenteritis was initiated. Eighteen days later, there were 36% of blasts noted on the blood film. Bone marrow trephine biopsy and molecular analysis revealed diffuse infiltration by AML (80% blasts) with mutated nucleophosmin 1. Conventional metaphase cytogenetic analysis showed a normal female karyotype in 17 of 20 metaphases, suggesting donor-derived leukemia. Treatment was initiated according to AMLSG-15-10 (low-dose cytarabine, etoposide, all-trans retinoic acid). Three weeks after diagnosis of AML, the patient died of severe sepsis in aplasia.
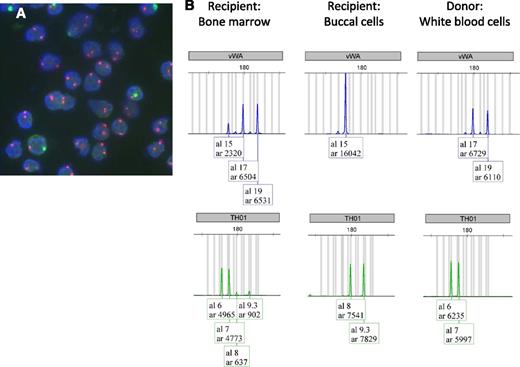
Donor origin of the leukemia was confirmed by X chromosome-specific fluorescent in situ hybridization (FISH) of the bone marrow (Figure 1A), and by short tandem repeat analysis of bone marrow and a buccal swab of the patient, as well as of stored leukocytes of the donor (Figure 1B and supplemental Table 2).
Donor origin of leukemia demonstrated by 2 different molecular methods. (A) Fluorescence in situ hybridization examination of the bone marrow demonstrating 85% of the cells to exhibit a XX chromosomal pattern (2 red signals per nucleus), all of them were morphologic with immature aspect, suggesting the leukemic cells of donor origin. Note the few residual cells of the recipient with XY chromosomal pattern (1 red and 1 green signal per nucleus). FISH was performed using the directly labeled, dual-color (red/green) X- and Y-chromosome probe mix (Xp11.1-q11.1/Yq12) Z-2016 (ZytoVision, Bremerhaven, Germany). The sections were processed with a paraffin pretreatment reagent kit (Abbott/Vysis, Baar, Switzerland), and hybridization was performed according to the manufacturer’s specifications. Denaturation was conducted for 10 minutes at 73°C, and the FISH probes were incubated overnight at 37°C in Hybrite (Abott/Vysis). Counterstaining was performed with 4,6-diamidino-2-phenylindole. The FISH signals were visualized on a Olympus BX43 fluorescence microscope equipped with double bandpass filters for simultaneous visualization of green and red signals. (B) Short tandem repeat profile of the 2 representative chromosomal loci vWA and TH01. Left: Recipient bone marrow cells at diagnosis of AML. Middle: Recipient buccal cells. Right: Donor white blood cells, demonstrating mixed chimerism and donor origin of cells. Taking all 8 discriminative chromosomal loci and the Amelogenin system into calculation, a donor chimerism of 86% can be demonstrated. This is in perfect agreement with the >80% blast infiltration of the marrow and 85% of cells exhibiting an XX chromosomal pattern.
Donor origin of leukemia demonstrated by 2 different molecular methods. (A) Fluorescence in situ hybridization examination of the bone marrow demonstrating 85% of the cells to exhibit a XX chromosomal pattern (2 red signals per nucleus), all of them were morphologic with immature aspect, suggesting the leukemic cells of donor origin. Note the few residual cells of the recipient with XY chromosomal pattern (1 red and 1 green signal per nucleus). FISH was performed using the directly labeled, dual-color (red/green) X- and Y-chromosome probe mix (Xp11.1-q11.1/Yq12) Z-2016 (ZytoVision, Bremerhaven, Germany). The sections were processed with a paraffin pretreatment reagent kit (Abbott/Vysis, Baar, Switzerland), and hybridization was performed according to the manufacturer’s specifications. Denaturation was conducted for 10 minutes at 73°C, and the FISH probes were incubated overnight at 37°C in Hybrite (Abott/Vysis). Counterstaining was performed with 4,6-diamidino-2-phenylindole. The FISH signals were visualized on a Olympus BX43 fluorescence microscope equipped with double bandpass filters for simultaneous visualization of green and red signals. (B) Short tandem repeat profile of the 2 representative chromosomal loci vWA and TH01. Left: Recipient bone marrow cells at diagnosis of AML. Middle: Recipient buccal cells. Right: Donor white blood cells, demonstrating mixed chimerism and donor origin of cells. Taking all 8 discriminative chromosomal loci and the Amelogenin system into calculation, a donor chimerism of 86% can be demonstrated. This is in perfect agreement with the >80% blast infiltration of the marrow and 85% of cells exhibiting an XX chromosomal pattern.
The kidney donor had died of intracranial hemorrhage after a head trauma. Medical workup prior to transplantation was unremarkable except for slight normocytic anemia (hemoglobin, 108 g/L) attributed to a knee replacement 1 week earlier. Spleen histology at autopsy was normal and the liver recipient of the same donor is leukemia free at the time of writing.
Kidney transplant recipients have a higher incidence of certain cancers.1,2 Almost all of these cancers are recipient in origin. Malignancies of donor origin are extremely rare. Most of them are donor-transmitted (ie, undetected donor malignancy is present in the transplanted organ). A few cases of donor-derived3 leukemia (ie, normal donor cells that develop into malignancy) have been reported in recipients of liver transplants.4,5 In the presented case, 3 disease mechanisms are possible: (1) hematopoietic progenitors that resided in the kidney at the time of transplant engrafted, despite full HLA mismatch, and underwent leukemic transformation; (2) a leukemic stem cell or clone was transplanted via kidney tissue; or (3) an abnormal hematopoietic cell differentiated from kidney tissue (so far, the kidney was considered to be an organ without hematopoietic capacity). Although all 3 hypotheses seem to be extremely unlikely, 1 of them has in fact substantiated in this patient. Due to the long interval between transplant and disease manifestation, the complete absence of signs of a pre-existent malignant hematologic disease of the donor, as well as the fact that the liver recipient of the same donor did not develop leukemia as of yet, we favor the first hypothesis.
Authorship
Contribution: S.G., J.P.H., and C.M.B. interpreted data; S.D. performed FISH; E.M., C.W., and P.A. took care of the patient; and S.G., J.P.H., C.M.B., S.D., J.R.P., E.M., C.W., and P.A. wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Christoph Bucher, Department of Hematology, University Hospital Basel, Petersgraben 4, Basel CH-4031, Switzerland; e-mail: christoph.bucher@usb.ch.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal