Abstract
Chronic granulomatous disease (CGD) is a rare inherited disorder due to a defect in NADPH oxidase, resulting in recurrent, life-threatening invasive infections and granulomatous inflammatory disorders. Although CGD is diagnosed mostly in early childhood, its prognosis has now much improved, allowing a majority of patients to reach adulthood. Very few studies have focused on the long-term outcome of adult CGD patients.
To study the clinical course and sequelae at various time points (age 16, 20, 30 and beyond) of CGD patients, diagnosed before 16 years of age.
A one-year (May 2012 to May 2013) French national retrospective study of CGD patients, diagnosed before the age of 16 years, and who had reached adulthood (defined as above 16 years of age) by the time of data collection. CGD patients were screened through the registry of the French national reference center of primary immune deficiencies (CEREDIH), and data were retrieved by reviewing medical charts and collected in a pre-defined case-report form.
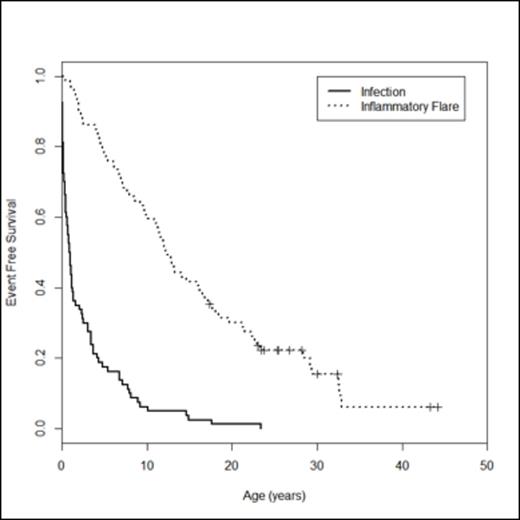
Eighty CGD patients (71 male (88.7%), 59 X-linked (73.7%), with a median NBT level of 0 [range:0; 15]) were included in the study. Median ages at diagnosis and last follow-up were 2.52 years [range: 0; 15.87] and 23.9 years [range: 16.61; 59.89], respectively. Seventeen patients (21%) were older than 30 years at time of last follow-up. Seven patients (8.8%) had undergone a hematopoietic stem-cell transplantation (HSCT). A total of 553 infections requiring hospital care (382 before age 16, and 171 thereafter), occurred among all patients during follow-up. The most common sites of infection were: pulmonary (31% of total infections, involving 77.5% patients), suppurative adenitis (24% of infections, 75% of patients), and cutaneous (16.2% of infections, 60% of patients). Aspergillus spp. (17%) and Staphylococcus aureus (10.7%) were the most common pathogens. These characteristics (sites and pathogens involved), as well as the annual frequency of infections, did not vary, when compared before and after age 16. When considering granulomatous events, a total of 224 inflammatory flares, mainly digestive (50%), pulmonary (16.7%) and urologic (10.3%), occurred among 71/80 (88.8%) patients. Thirty autoimmune events (mainly discoid lupus erythematosus) also occurred among 14/80 patients (17.2%). The median age of the first inflammatory event (12.5 years [range: 0.25; 44.2]) was much higher than that of the first serious infectious event (0.97 years [range: 0; 23.9]) (figure 1). The annual frequency of inflammatory events did not however significantly increase after age 16. Concerning the long-term consequences of such repeated infectious and steroid-treated inflammatory events, the main sequelae in CGD adults were a small adult median height and weight (167.5cm [range: 138; 185] and 56 kg [range: 35; 90] at age 20), as well as mild chronic restrictive respiratory failure (26.7% of chronic dyspnoea at the age of 30 years). At the age of 16 years, only 58% of patients were in high school. After 30 years, 9/13 (69%) patients were working, and 2 had had children. Ten patients died during adulthood at a median age of 23.6 years [range: 18.2; 45.4], most of them of infectious causes.
Adult CGD patients display similar characteristics and rates of severe infections as during their childhood. As CGD patients grow older, inflammatory flares also become a major concern, because of an older age of appearance. The high rate of handicap that these repeated infectious and inflammatory events entail in adult CGD patients, now becomes a matter of medical and social considerations. A careful follow-up is thus recommended in specialized centers. Finally, HSCT and gene therapy should be more systematically considered in order to try to avoid long-term complications, which are responsible for major disabilities.
Infection-free and inflammatory flare-free survival curves in 80 French CGD patients having reached an adult age.
Infection-free and inflammatory flare-free survival curves in 80 French CGD patients having reached an adult age.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal