Abstract
We describe here platelet response and remission observed with romiplostim treatment in patients with ITP.
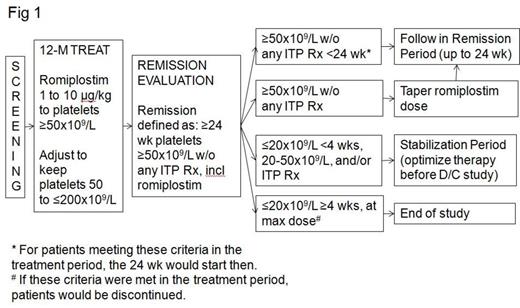
Patients with an ITP diagnosis for less than 6 months who received first-line therapies only (ie, corticosteroids, IVIG, anti-D) received QW romiplostim for up to 12 months in the treatment period (Fig 1). The primary objective was to describe the number of months with a platelet response during the 12-month treatment period; secondary objectives included incidence of ITP remission and splenectomy. The romiplostim dose was increased QW by 1 μg/kg from 1 μg/kg up to 10 μg/kg to reach a platelet count of ≥50x109/L, adjusting to maintain a platelet count of 50-200x109/L. Patients who maintained platelet counts ≥50x109/L on romiplostim only entered a dose-tapering period in which the romiplostim dose was decreased by 1 μg/kg Q2W as long as platelet counts remained ≥50x109/L. Starting when the dose tapered to 0 during either the 12-month treatment period or at the end of the dose-tapering period, patients were followed to determine whether they had ITP remission (24 weeks platelet counts ≥50x109/L without any treatment for ITP, including romiplostim). At the end of 12 months, patients who 1) had platelet counts ≤20x109/L for <4 consecutive weeks, 2) had platelet counts of 20-50x109/L, and/or 3) were receiving treatment for ITP besides romiplostim had the option to enter a stabilization period (≤8 weeks) while the investigator determined suitable post-study therapy. Patients with platelet counts ≤20x109/L for ≥4 consecutive weeks on the highest romiplostim dose were discontinued from the study for non-response. Interim data up to March 2013 are reported here.
Of the patient population (N = 71), 59.2% were women, median (Q1, Q3) age was 37 (28, 56) years, median (Q1, Q3) time since ITP diagnosis was 2.2 (0.9, 4.4) months, and median (Q1, Q3) platelet count at screening was 20 (12, 25) x109/L. Past treatments included steroids (96%), IVIG (42%), and anti-D (1%). Prior to the study, platelet transfusions were received by 9% of patients. 30 patients (42%) completed treatment, 31 (44%) are continuing treatment, and 10 (14%) discontinued romiplostim (due to consent withdrawn n = 2, adverse event n = 3, requirement for alternative therapy n = 3, lost to follow-up n = 1, death n = 1). Patients had a median (Q1, Q3) of 51 (34, 52) weeks of treatment with a median (Q1, Q3) average QW dose of 2.1 (1, 3.8) μg/kg. 66 (93%) patients had a peak platelet count ≥50x109/L. The median (Q1, Q3) time with a platelet response was 9 (6, 12) months; the median (95% CI) time to platelet response was 2.1 (1.1, 3.1) weeks; platelet counts are in Fig 2. Of 38 evaluable patients (ie, known remission status), 11 (29%, 95% CI 15% to 46%) had ITP remission. One patient had a splenectomy and 6 had treatment failure (defined as platelet count ≤20x109/L for 4 consecutive weeks at 10 μg/kg QW, requirement of alternative therapy, or death). Of the 71 patients receiving romiplostim, 9 patients had serious adverse events (2 treatment-related: 1 case each of gastritis and increased transaminases). There were also 3 adverse events leading to discontinuation of romiplostim (non-Hodgkin's lymphoma, leukocytosis, and the aforementioned increased transaminases, these last 2 treatment-related). Other serious adverse events, also occurring in 1 patient each, included atrial fibrillation, dapsone syndrome, fecaloma, the aforementioned non-Hodgkin's lymphoma, pleuritic pain, and tendon rupture. There were no fatalities reported as adverse events; the death leading to discontinuation was due to cerebral hemorrhage which began before the patient received romiplostim. The most common adverse events were headache (17%), arthralgia (13%), and nasopharyngitis (10%). The most common hemorrhage adverse events were hematoma (7%), petechiae (7%), and epistaxis (7%). No bone marrow findings were reported.
In this trial, patients with an ITP diagnosis for less than 6 months treated with romiplostim had a high response rate (over 90%), with platelet responses occurring quickly (median time to response of 2 weeks) and median number of months with a platelet response of 9 months. To date, 29% of evaluable patients have shown remission (24 weeks of platelet counts ≥50x109/L without any ITP treatment). There were no new safety signals. Updated data from this ongoing study will be presented in the future.
Stasi:Amgen: Honoraria, Speakers Bureau; GSK: Honoraria, Speakers Bureau; Genzyme: Honoraria, Speakers Bureau; Suppremol: Consultancy. Newland:Geron: Consultancy; Amgen: Membership on an entity’s Board of Directors or advisory committees, Research Funding, Speakers Bureau; GSK: Membership on an entity’s Board of Directors or advisory committees, Research Funding, Speakers Bureau; Octapharma: Research Funding. Godeau:Amgen: Consultancy, Membership on an entity’s Board of Directors or advisory committees; Roche: Consultancy, Research Funding; GSK: Consultancy; LFB: Consultancy. Jia:Amgen: Employment, Equity Ownership. Lopez:Amgen: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal