Abstract
PET/CT is a reliable technique for assessing skeletal involvement in MM and a valuable tool at the onset of the disease for predicting outcomes in those patients who are eligible to subsequently receive autologous stem cell transplantation (ASCT). However, the prognostic role of PET/CT after treatment and/or during the follow up of the disease, as well as in the non ASCT setting, still remains less defined. To address these issues, we retrospectively analyzed 282 symptomatic MM pts, with a median age of 58 yo, (range 22-83), who were diagnosed and treated in a single institution between 2002 and 2012, and were followed for a median of 66 months. Treatment included ASCT in 70%, novel agents in 77% and was bortezomib-based in 37% of the cases. All the pts were studied with PET/CT at baseline, then every 12-18 months during follow-up, and at the time of each subsequent relapse; for 189 of them PET/CT scans at baseline and 3 months after the end of first line treatment were available. Bone marrow involvement was described as negative, diffuse or focal. The number of focal lesions (FLs), their associated standardized uptake value (SUVmax) and presence of extra-medullary disease (EMD) were recorded. Forty two percent of the pts at diagnosis had > 3 FLs and in 50% of them SUVmax was > 4.2; EMD was present in 5% of the cases. On multivariate analysis, these 3 variables adversely affected PFS and OS, and retained prognostic relevance independently of the treatment received (including or not ASCT, bortezomib- or non-bortezomib-based). On multivariate analysis, ISS stage 3, presence of >3 FLs at PET/CT and failure to achieve CR during or after first line treatment were the leading factors independently associated with shorter PFS and OS. These 3 variables enabled the definition of a scoring system, based on the number of risk factors simultaneously present (score 0: none of the 3 adverse factors, 31% of the pts; score 1: only one out of the 3, 37%, score 2+: 2 or 3 factors, whatever of them, 32% ), that predicted for PFS and OS. More specifically, median PFS was 36 months (mos) for pts with score 0, 58 mos for score 1 and 74 mos for score 2+ (P=0.000). OS was also significantly influenced by the number of adverse factors, with a progressive increase in hazard ratios. A similar stratification into 3 prognostic groups was obtained when SUVmax > 4.2 and presence of EMD replaced FLs>3 within the scoring system.
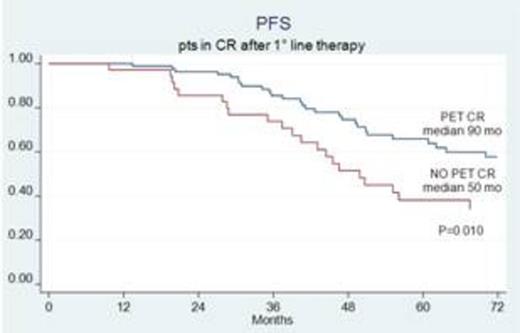
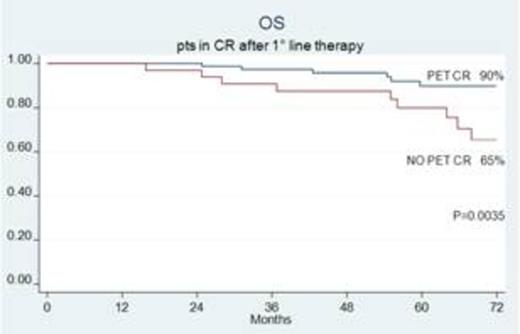
After treatment, PET/CT negativity (PET-CR) was observed in 70% of the pts, while conventionally-defined CR was achieved in 53% of them. Attainment of PET-CR favorably influenced PFS and OS, both in uni and multivariate analyses. Notably, 29% of the pts who achieved CR according to conventional criteria still had positive PET/CT scans: their median PFS was 50 mos as compared with 90 mos for those pts who also achieved PET-CR (P= 0.01) (fig. 1). OS was significantly inferior, as well, for pts not achieving PET-CR, with 6-year estimate of 65% in comparison to 90% for PET negative pts (P=0.0035) (fig. 1). On multivariate analysis, PET-CR was an independent factor predicting for prolonged PFS (P= 0.004) and OS (P= 0.02) within the conventionally-defined CR group.
Sixty three percent of the pts experienced relapse or progression, after a median of 56 mos from the end of first-line treatment. In 37% of them, progression was only serological, both serological and skeletal in 48%, only skeletal in 15% and in 12% of these latter patients it was exclusively detected by systematic PET/CT during the follow-up (no pain or pathological fractures). A logistic regression analysis of baseline and post treatment features revealed that persistence of SUVmax > 4.2 after the end of first line treatment was independently associated with exclusive PET/CT progression.
In conclusion, PET/CT was confirmed as a reliable predictor of outcome in newly diagnosed MM pts, whatever the treatment. PET/CT combined with ISS stage and attainment of CR to first line therapy was able to split pts in different prognostic groups. Importantly, PET/CT contributed to a more careful and deep evaluation of CR, going beyond the conventionally defined level, and should thus be recommended as a complementary tool to define “true” CR. Finally, in pts with a persistent high glucose metabolism after first line treatment, PET/CT can be recommended during the follow-up, in order to point out possible progression, not otherwise identifiable.
Zamagni:Celgene: Honoraria; Janssen-Cilag: Honoraria. Cavo:Celgene: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees; Janssen: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees; Millennium: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees; Onyx: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees; Bristol-Myers Squibb: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal