Abstract

Arthropathy, the most costly chronic complication of severe hemophilia A (HemA) can be prevented by routine replacement of factor VIII (FVIII) when initiated prior to joint bleeding (primary prophylaxis) [NEJM;357:535]. However, the efficacy of prophylaxis initiated after the onset of recurrent hemarthroses or with established arthropathy (secondary or tertiary prophylaxis) is unknown. This individual patient meta-analysis was performed to derive the natural history of arthropathy in HemA patients treated only in response to acute bleeding (on demand therapy) as a baseline for future work to estimate the amelioration of arthropathy attributable to secondary or tertiary prophylaxis.
Data from individual participants in 3 studies who received on demand therapy were aggregated into a single database. Eligibility for this analysis included FVIII ≤ 2%, negative history for inhibitor, bleeding history for 12 months prior to study data acquisition and assessment of both ankles, knees and elbows; joints were assessed using physical examination (PE) and T2* gradient echo MRI scored as previously described using the World Federation of Hemophilia Gilbert score and the 45 point extended MRI scales [Haemophilia;6:649; ISTH OP Mon 7/1/13, 9 am]. MRI data were divided into soft tissue and osteochondral changes. Bleeding and Gilbert data for all 6 joints and MRI data for knees and ankles were analyzed using standard descriptive statistics and regression methods to quantify the rate of change in scores of joint damage with age.
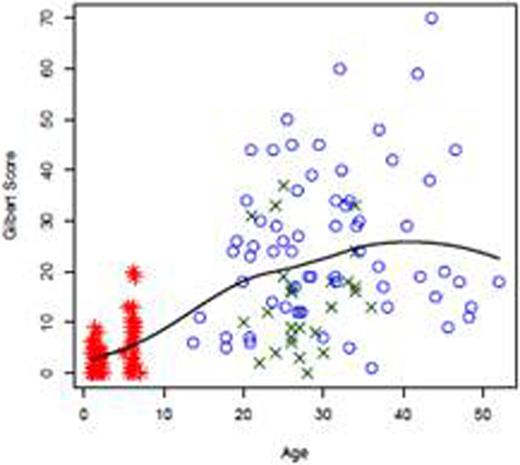
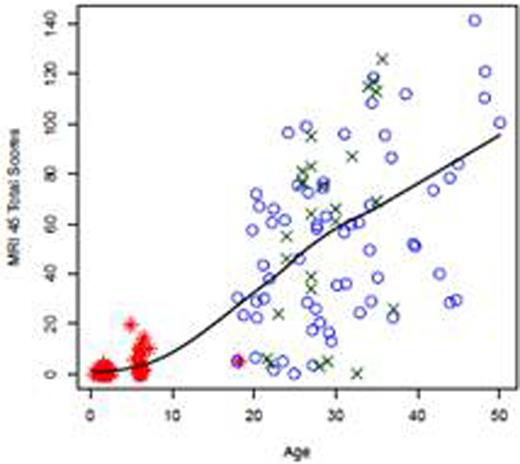
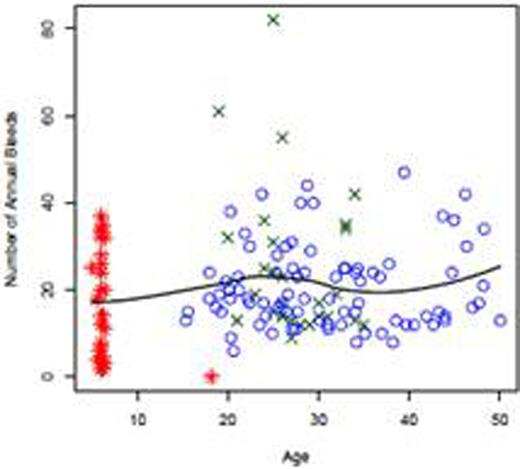
The 3 studies included the Joint Outcome Study [NEJM;357:535] and the JOS Continuation Study (JOSc), the Spinart Study baseline results [JTH;11:1119] and a Cross-Sectional MRI study [Haemophilia;189 Suppl3:117]. The 3 studies provide data on 275 individuals aged 1 to 50 years. Clinical, Gilbert and MRI data were extracted and analyzed from multiple joints in each of 157 individuals who were receiving on-demand treatment only. The median age was 21 (range 1 – 50), and across all studies the median number of bleeding episodes in the prior 12 months was 18 (range 0 to 82). The rate of change in outcomes as a function of age is shown in Table 1 and Figure 1. The number of bleeding episodes was approximately constant at 20 bleeding episodes per year regardless of age (Figure 1a; p = 0.72 for relationship with age). Gilbert scores showed a steeper rise in young patients but did not increase after the late teens (Figure 1b; change of 0.34 Gilbert points/year of life, p=0.07).
Rate of change (β1) in joint outcomes as a function of age in severe HemA treated with on demand therapy.
| Outcome . | n . | β1*(Slope) . | 95% CI . | P-Value . |
|---|---|---|---|---|
| Bleeding events/year | 112 | -0.0488 | (-0.3227, 0.2251) | 0.7247 |
| Gilbert Joint PE Score | 92 | 0.3355 | (-0.0221, 0.6931) | 0.0656 |
| MRI Total Score | 90 | 2.0438 | (1.1731, 2.9145) | < 0.0001 |
| MRI Bone & Cartilage Score | 90 | 1.9609 | (1.187, 2.7348) | < 0.0001 |
| MRI Soft Tissue Score | 90 | 0.0829 | (-0.068, 0.2338) | 0.2781 |
| Outcome . | n . | β1*(Slope) . | 95% CI . | P-Value . |
|---|---|---|---|---|
| Bleeding events/year | 112 | -0.0488 | (-0.3227, 0.2251) | 0.7247 |
| Gilbert Joint PE Score | 92 | 0.3355 | (-0.0221, 0.6931) | 0.0656 |
| MRI Total Score | 90 | 2.0438 | (1.1731, 2.9145) | < 0.0001 |
| MRI Bone & Cartilage Score | 90 | 1.9609 | (1.187, 2.7348) | < 0.0001 |
| MRI Soft Tissue Score | 90 | 0.0829 | (-0.068, 0.2338) | 0.2781 |
Estimated slope from linear regression of outcome on age (analyses exclude JOS/JOSc data in order to estimate the rate of change in adults).
Number of bleeding episodes in prior 12-months (1a), Gilbert score (1b) and MRI total score (1c) as a function of age among patients on episodic treatment of hemophilia. Meta-analysis of 3 studies: red*(JOS/JOSc), greenX (X-sectional) and blue °(Spinart).
Number of bleeding episodes in prior 12-months (1a), Gilbert score (1b) and MRI total score (1c) as a function of age among patients on episodic treatment of hemophilia. Meta-analysis of 3 studies: red*(JOS/JOSc), greenX (X-sectional) and blue °(Spinart).
MRI scores, in contrast to bleeding rates and Gilbert scores, showed continued age-related deterioration (Figure 1c; change of 2 MRI points/year of life, p < 0.0001). Age-related total and osteochondral deterioration on MRI increased steadily with age (on average 2 MRI-points/year of age, p < 0.0001 for each), whereas soft tissue scores increased rapidly to approximately 9 by age 20, and then plateaued at a score of approximately 10 for ages 20-50 (0.08 MRI points/year, p =0.28).
Individual patient meta-analysis of bleeding frequency, joint PE and MRI joint structure was useful to determine the natural history of hemophilic arthropathy in patients treated with on-demand therapy, and showed a continuous increase in joint bone and cartilage abnormalities across the age span despite an early leveling in bleeding rate and joint physical function. These data will be critical to determine the quantitative effects of prophylaxis on mitigation of joint deterioration when initiated at various ages following the onset of joint bleeding.
Manco-Johnson:Bayer HealthCare: Research Funding. Lundin:Bayer HealthCare: Research Funding. Hong:Bayer HealthCare: Employment. Oldenburg:Octapharma AG: Consultancy, Investigator Other. Manco-Johnson:Biogen Idec: Membership on an entity’s Board of Directors or advisory committees; Baxter BioScience: Membership on an entity’s Board of Directors or advisory committees; CSL Behring: Membership on an entity’s Board of Directors or advisory committees, Research Funding; Bayer HealthCare: Membership on an entity’s Board of Directors or advisory committees, Research Funding; NovoNordisk: Membership on an entity’s Board of Directors or advisory committees; Eisai: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal