Abstract
Neurovascular sequalae are a common occurrence in Sickle Cell Anemia (SCA), with 11% of patients suffering cerebral vascular accident (CVA), or overt stroke by their twentieth birthday and 40% of patients developing silent cerebral infarcts (SCI) by age 14. Elevated transcranial Doppler (TCD) velocity of the middle cerebral artery identifies patients at risk for stroke, and this risk can be reduced by chronic transfusion therapy. However, the specificity of TCD is low causing many patients to be transfused unnecessarily. To further refine cerebrovascular risk stratification, we are studying factors responsible for normal and pathophysiologic cerebral blood flow (CBF) in SCD patients. Cerebral blood flow is increased in SCA patients compared to controls, but is believed to be a compensatory mechanism for chronic anemia and systemic desaturation. In order to test this hypothesis, we studied whole CBF and oxygen delivery (DO2) at rest and in response to hyperoxia in subjects with SCA and sickle cell trait (SCT).
All patients were recruited at Children's Hospital Los Angeles through an IRB approved protocol. Informed consent was obtained for all patients. Exclusion criteria included pregnancy, previous stroke, acute chest or pain crisis hospitalization within one month. EKG, peripheral arterial oxygen saturation (SaO2), and fractional inspired oxygen (fiO2) were measured continuously throughout the study. Imaging consisted of a survey, reference scan, angiography localization, and nine axial phase contrast (PC) images. PC slices were placed inferior to the Circle of Willis, perpendicular to the carotids and basilar arteries. Participants received room air and 100% O2 through a non rebreathing respiratory circuit at 10 L/m. Room air exposure 20 minutes with six PC images collected throughout. Oxygen was delivered for 5 minutes followed by three more PC images. Blood for hemoglobin (HGB) and hematocrit (HCT) were drawn prior to MRI testing. No adverse events were reported upon follow up.
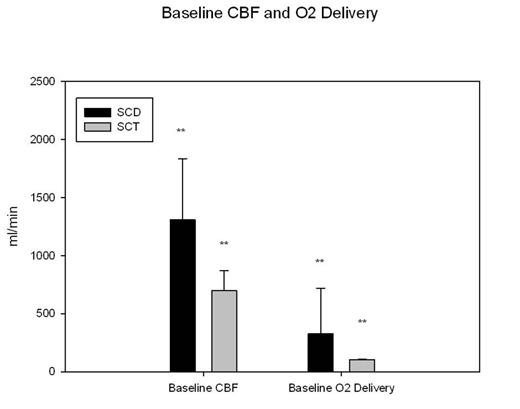
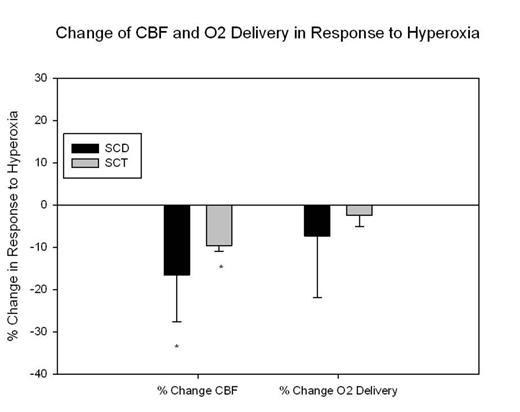
Nine patients with SCA (5 male, 22.5 ± 6.7 yo p<0.05) and 3 with sickle cell trait (2 male, 36.7 ± 8.7 yo p<0.05) were studied. Baseline HGB was 25% lower (9.7 ± 1.3 versus 12.9 ± 0.1) and baseline HCT was 41% lower (28.0 ± 3.6 versus 47.3 ± 0.14 SCT) in SCA patients (p<0.05). Baseline whole brain CBF was elevated in SCA (1398 ± 400 ml/min versus 700 ± 172 ml/min). After correcting for HGB and SaO2, DO2 remained higher in SCA (192 ± 75 ml/min versus 105 ± 1.4 ml/min, p<0.05). During hyperoxia, whole brain CBF decreased by 10-15%, but the change was proportional to increased oxygen carrying capacity such that there was no change in DO2 in either populations.
The increase in CBF we observed in SCA patients has been described using other modalities. However, we are the first to demonstrate that the increased flow observed is almost double what can be explained by their anemia and arterial desaturation alone. There are several possibilities for this observation. 1) SCA patients could have increased cerebral metabolic rate. If so, their mixed cerebral venous saturation will be normal and the flow is appropriate; 2) SCA patients have a mismatch between cerebral perfusion and metabolic demand, whether much of the increased flow does not effectively unload oxygen. If so, cerebral venous saturation would be high. We are currently optimizing MRI and NIR's technologies to estimate cerebrovascular metabolic rate, mixed cerebral venous saturation, and local supply-demand balance.
Baseline CBF and O2 delivery in SCA and control group. ** statically significant population difference
Baseline CBF and O2 delivery in SCA and control group. ** statically significant population difference
Responce to 100% oxygen exposure. *statistically significant change from baseline
Responce to 100% oxygen exposure. *statistically significant change from baseline
Coates:Novartis Inc.: Honoraria, Speakers Bureau; Apopharma: Honoraria, Speakers Bureau; Shire: Speakers Bureau. Wood:Shire: Consultancy, Research Funding; Apopharma: Honoraria, Patents & Royalties; Novartis: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal