Abstract
Disseminated intravascular coagulation (DIC) is a lethal complication in patients with hematological malignancies. Although standard therapy against DIC remains to be established, soluble recombinant thrombomodulin (rTM), which serves as a receptor for thrombin, has been developed and its effectiveness for DIC was reported (Saito et al, J Thromb Haemost 2006). However, there is not enough evidence of rTM on DIC associated with hematological malignancy. Therefore we retrospectively compared outcome of hematological malignancy-related DIC treated with rTM or other conventional anticoagulant therapies.
One hundred and sixty-five consecutive DIC episodes in 146 patients with hematological malignancies (AML except for APL, 49; APL, 21; ALL, 19; NHL, 31; myeloma, 11; CML, 7; other; 8) hospitalized between January 2004 and May 2013 in University of Tsukuba Hospital were retrospectively analyzed. Diagnosis of DIC was based on DIC score of Japanese Ministry of Health and Labor Welfare criteria (Kobayashi et al, Bibl Haematol 1983). DIC was induced by hematological malignancy itself (h-DIC) or severe infection secondary to hematological malignancy (i-DIC) in 108 and 57 episodes, respectively. In 73 episodes, 380 units/kg/day of rTM was administered intravenously from the onset of DIC for median of 6 (range, 2-22) days. Other DIC episodes were treated with conventional anticoagulant therapy (low molecular weight heparin, 65; gabexate mesilate, 17; other anticoagulant, 10). Every anticoagulant therapy was accompanied by treatment for DIC-causing disease. We compared recovery time from DIC (the day when DIC score was decreased to 5 or less), overall survival, and severe hemorrhagic events related to the treatment, between rTM- and conventional anticoagulant-treated groups.
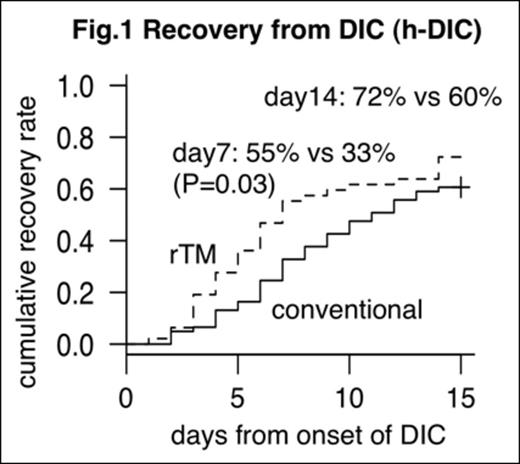
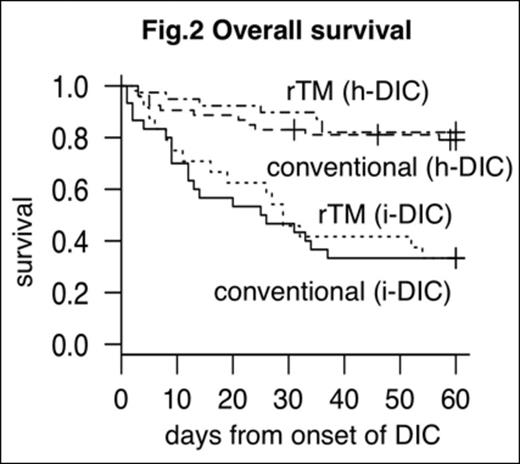
Fifty-three DIC episodes were accompanied by bleeding tendency at the onset. In h-DIC, recovery from DIC was significantly more prompt in rTM-treated group, with the recovery rates of 55% (95% CI: 40 - 68) in the rTM-treated group and 33% (95% CI: 21 - 45) in the conventional therapy group at day 7 after the therapy initiation (P = 0.03, Fig.1). On day 14, the recovery from h-DIC was seen in 72% (95% CI: 56 - 83) and 60% (95% CI: 47 - 71) with the rTM and conventional therapies, respectively (P = 0.2). By contrast, recovery from i-DIC was significantly worse than that from h-DIC, and was not influenced by anticoagulant therapies. Recovery rates from i-DIC at day 14 were 27% (95% CI: 12 - 45) in the rTM-treated group and 36% (95% CI: 19 - 52) in the conventional therapy group (P = 0.6). Day 60 overall survival rates in h-DIC were 82% (95% CI: 66 - 91) and 79% (95% CI: 65 - 88) in the rTM-treated and conventional therapy groups. In i-DIC, on the other hand, 33% (95% CI: 16 - 52) and 33% (95% CI: 18 - 50) survived with the rTM and conventional therapies, respectively (Fig.2). Severe hemorrhagic events that led to discontinuation of anticoagulant therapy was significantly less in the rTM-treated group (3%; 95% CI, 0.3 - 9) compared with that in the conventional therapy group (12%; 95% CI: 6 - 20; P = 0.04).
The recovery from h-DIC treated with rTM was more prompt compared to that with conventional anticoagulant therapy. Although the conventional anticoagulant therapy has fostered bleeding tendency, bleeding tendency was reduced after rTM administration in most of the DIC episodes. We emphasize that rTM can be an effective anti-DIC agent without causing adverse hemorrhagic event even in DIC cases with preexisting bleeding tendency. However, the outcome was still significantly worse in i-DIC secondary to hematological malignancies even after introduction of rTM. Further development of anticoagulant therapy is required for the control of i-DIC.
Chiba:Asahi Kasei Pharma: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal