Abstract
Philadelphia chromosome positive (Ph+) acute lymphoblastic leukemia (ALL) is characterized by t(9;22) and is associated with poorer outcomes. Ph+ ALL responds initially to conventional chemotherapy but overall survival (OS) is low at < 20% with no curative form of post-remission chemotherapy. Allogeneic hematopoietic stem cell transplantation (HSCT) in first remission has historically been the only curative treatment modality, yet only cures approximately 30% of patients, typically in younger patients (less than 60 years of age). The introduction of tyrosine kinase inhibitors (TKIs) that target the fusion protein Bcr-ABL have altered the management of Ph+ ALL, with durable remission of 40-50%. Debate remains over the optimal chemotherapy “backbone” to combine with TKIs in the treatment of Ph+ ALL, given outcomes reported using nonmyeloablative approaches (Foà R, et al. Blood 2011; 118:6521).
We conducted a single-center, retrospective analysis of patients with newly diagnosed Ph+ ALL treated with various induction regimens in combination with TKIs. Patients aged 18 or older were included and comparisons were made between regimens considered to be intensely myelosuppressive (IMS) (i.e. hyperCVAD or ALL-2) and regimens considered less myelosuppressive (LMS) (i.e. ECOG 2993, L-20, or vincristine ± corticosteroids). The primary endpoint was a comparison of overall survival between treatment groups. Secondary endpoints included assessment of complete remission (CR) rates, disease free survival (DFS), likelihood to proceed to allogeneic HSCT, the effect of HSCT on overall survival, and hematologic and non-hematologic toxicities.
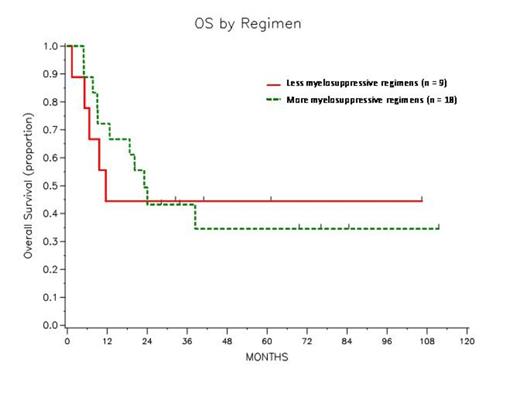
Twenty-seven patients were included in this analysis. In combination with imatinib or dasatinib, eighteen patients were treated with IMS regimens while nine patients received LMS regimens. The groups were well-matched in baseline characteristics other than age (median: IMS - 49.6 years old vs. LMS -70.6 years old, p = 0.022). CR rates were high in both treatment groups (IMS - 94.4% vs. LMS -88.9%). No difference was observed in overall survival between the groups (3-year OS rate: IMS - 43.2% vs. LMS - 44.4%, Log-rank p = 0.921). There was a nonsignificant difference in DFS for patients favoring with IMS regimens (3-year DFS rate: IMS -43.2% vs. LMS - 33.3%, Log-rank p = 0.606). Patients treated with IMS regimens were more likely to proceed to transplant in CR1 [IMS - 88.2% (n = 15/17) vs. LMS - 22.2% (n = 2/ 9), p = 0.002). When evaluating the impact of HSCT on 3-year OS using a landmark analysis of 6 months post-induction therapy there was no difference between 13 patients who proceeded to HSCT compared to the 9 who did not (3-year OS rate post landmark: Yes HSCT - 33.7% vs. No HSCT - 55.6%, Log-rank p = 0.4). Overall, the toxicity during induction was similar in both treatment groups despite the increased myelosuppression that was expected in the more intense treatment group (100% experience grade 3 or greater hematologic toxicity vs. 89.9%). Among patients who achieve ANC>1000, those receiving LMS regimens did have a decrease in time to achieve this benchmark, though statistically it was not significant (median: 16 days vs. 21 days, p = 0.243).
While limited by the small sample size, it appears that the combination of TKIs with either IMS or LMS treatment regimens will achieve high CR rates. In our study OS was improved compared to historical controls prior to the introduction of TKIs and this includes a number of patients who did not undergo HSCT (Fielding AK, et al. Blood 2009; 113:4489-4496). It appears that in older patients who receive LMS regimens may not have inferior outcomes compared to younger patients who received IMS despite being far less likely to undergo HSCT in CR1. This finding may potentially prove to be significant given that up to 50% of patients with ALL older than 60 years of age are Ph+.
Summary of results comparing intensely myelosuppressive regimens vs. less myelosuppressive regimens
 |
 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal