Abstract

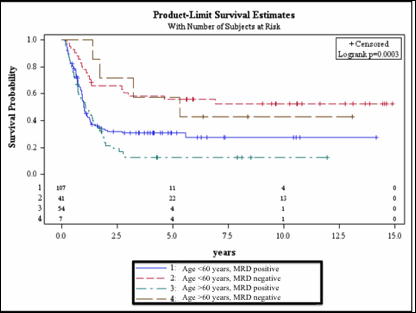
Although the therapy of acute myeloid leukemia (AML) has remarkably improved over the last 2-3 decades, two thirds of young adults still die of their disease. In elderly adults, who represent the majority of patients with AML, the results are even more unsatisfactory with less than 10% of patients being long-term survivors. Based on this, age is universally recognized as a critical prognosticator affecting outcome and therefore treatment choice. In consecutive series of adult patients with de novo AML, we have repeatedly demonstrated the prognostic role of minimal residual disease (MRD) as detected by flow cytometry. In particular, we have found that a level of MRD ≥ 3.5x10e-4 residual leukemic cells (RLC) at the end of consolidation is associated with a relapse rate of 70-80%. In the present study we evaluated whether the prognostic impact of MRD assessment after consolidation remained unaltered even in age-stratified (< 60 and > 60 years) populations of adult patients with de novo AML. To this end, we analyzed 149 young (median age 46, range 18-60) and 61 elderly adults (median age 67, range 61-78). All patients under study achieved complete remission after an induction therapy of the EORTC/GIMEMA protocols AML10, LAM99P and AML12 (for patients < 60 years) or AML13, AML15A and AML17 (for patients > 60 years). The two cohorts were well balanced in terms of frequency of FLT3-ITD and NPM1 mutated cases. A lower frequency of favorable-risk karyotypes was observed in elderly versus young patients (4% vs 19%, p=0.024). Of 149 younger patients, 105 (70%) underwent stem cell transplantation (SCT) (45 allogeneic, 60 autologous) as compared to 7 (11%) in the older age group (1 allogeneic, 6 autologous), (p=<0.0001). The frequency of MRD negative measurements was lower among elderly patients as compared to the younger ones [7/61 (11%) vs 42/146 (28%), p=0.009]. The median value of MRD after induction was 2.9x10e-3 RLC (range 0-170) and 3.1x10e-3 RLC (range 0-220) in younger and older patients (p=NS), respectively. Conversely, post-consolidation MRD levels were significantly lower in the younger cohort (1.7x10e-3 RLC, range 0-360) as compared to the older one (3.3 x10e-3 RLC, range 0-72), (p=0.018). In both age groups, disease-free survival (DFS) (Fig. 1) and cumulative incidence of relapse (CIR) were significantly longer and lower for patients who achieved MRD negativity at the post-consolidation time-point (p=0.0003 and <0.0001, respectively). In multivariate analysis, MRD at the post-consolidation time-point (p=0.0013) and karyotype (favorable vs adverse, p=0.0073; intermediate vs adverse, p=0.06) confirmed an independent prognostic role affecting DFS. Even SCT procedure (both autologous or allogeneic), analyzed as a time-dependent covariate, was significantly associated to DFS (p<0.001). Age did not score as a significant variable in any prognostic model. In conclusion, elderly adults with AML infrequently become flow-MRD negative after consolidation therapy (11% vs 29%, p=0.008), likely due to a less intensive approach. However, those who succeed to enter MRD negativity have significantly superior DFS and CIR – comparable to the ones of young patients - that than those who remain positive.Close modal
Figure 1
Disease free survival stratified according to age and MRD status.
Figure 1
Disease free survival stratified according to age and MRD status.
Disclosures:
No relevant conflicts of interest to declare.
Author notes
*
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract
© 2013 by The American Society of Hematology
2013

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal