Abstract

Based on CALGB trial in 1994, 3-4 cycles of high-dose cytarabine have been one of the standard consolidation therapies. Despite the confirmed efficacy of anthracyclines for remission induction, the role of anthracyclines for postremission consolidation is a subject still under debate. In this retrospective analysis, we compared the efficacy of high-dose cytarabine (>=1.5 g/m2) and intermediate-dose cytarabine (1 g/m2) combined with anthracyclines as postremission therapy.
The patients enrolled in the Korea University AML registry from September 2002 to August 2011 were analyzed. Inclusion criteria were as follows; 1) Complete remission was achieved in first induction by standard 3+7 regimen (idarubicin 12 mg/m2 or daunorubicin 45 or 60 or 90 mg/m2 on D1-3 + cytarabine 100 mg/m2 on D1-7) 2) Postremission therapy was performed for 3-4 cycles by one of the following regimen; Arm A (high-dose cytarabine): cytarabine 3 g/m2 for patients =< 60 years old or 1.5 g/m2 for patients > 60 years old, q 12 hours on D1, 3, 5. Arm B (intermediate-dose cytarabine combined with anthracyclines): cytarabine 1.0 g/m2 q 12 hours on D1-3 combined with mitoxantrone or idarubicin 12 mg/m2 on D1,2. Univariate and multivariate analysis for survival were performed by Kaplan-Meier and Cox-regression analysis, respectively.
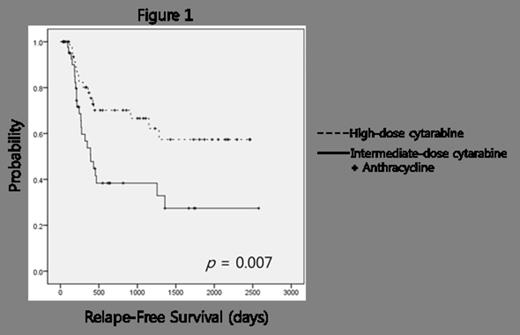
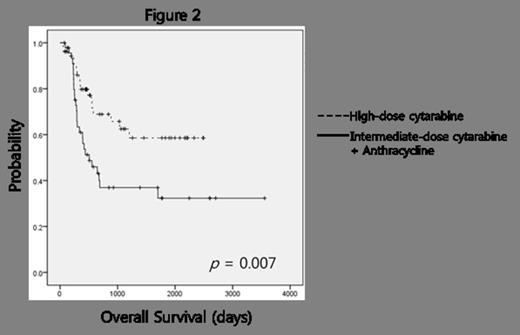
Among 172 AML patients enrolled in the registry, 95 patients (55%) were satisfactory for inclusion criteria. The number of arm A and B was 51 and 44, respectively. Some patients (N=47) with intermediate or high-risk cytogenetics have undergone autologous or allogeneic stem cell transplantation. Univariate analysis for relapse-free survival (RFS) demonstrated that age (=< 60 vs. >60, p=0.007), stem cell transplantation (p=0.001), and consolidation regimen (Arm A vs. Arm B, p=0.007) were statistically significant. The median RFS of arm A was not reached and significantly superior to that of arm B (14.0 months, 95% CI 8.5 months to 19.5 months) (Figure 1). Multivariate analysis showed that stem cell transplantation (HR 0.384, 95% CI 0.195 to 0.758, p=0.06) and consolidation regimen (HR 0.454, 95% CI 0.237 to 0.872, p=0.018) were independently significant factors for RFS. With regard to overall survival (OS), age (p<0.001), performance status (ECOG 0,1 vs. 2,3, p<0.001), WBC count at diagnosis (<20000/μL vs. >=20000/μL, p=0.033), WHO classification (de novo vs. secondary, p=0.05), stem cell transplantation (p=0.001), and consolidation regimen (p=0.007) were statistically significant by univariate analysis. The median OS of arm A was also not reached and significantly superior to that of arm B (18.1 months, 95% CI 7.7 months to 28.5j months) (Figure 2). Multivariate analysis for OS showed that age (HR 0.482, 95% CI 0.248 to 0.939, p=0.032), stem cell transplantation (HR 0.469, 95% CI 0.244 to 0.899, p=0.023), and consolidation regimen (HR 0.474, 95% CI 0.252 to 0.894, p=0.021) were independently significant factors. There was no statistical significance in treatment-related mortality between arm A and arm B (7% and 4%, respectively, p=0.541).
This analysis showed that as compared with intermediate-dose cytarabine (1.0 g/m2) combined with anthracyclines, high-dose cytarabine consolidation (>=1.5 g/m2) was independently favorable factor for both RFS and OS in AML patients who had achieved complete remissions in first induction by standard 3+7 regimen. Based on this study, we hypothesize that the addition of anthracycline during consolidation might have a limited value as compared with cytarabine intensification. The confirmatory prospective trial should be required.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal