Abstract
Limited data exist with respect to outcome and optimal therapeutic strategies in patients with central nervous system (CNS) involvement in multiple myeloma (MM). We present a single center experience of patients with myelomatous CNS involvement in newly diagnosed and relapsed / refractory MM.
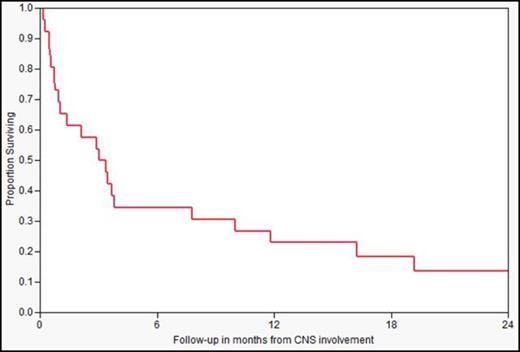
Of 4060 patients with MM seen at Mayo Clinic, Rochester, MN between January, 1st 1998 and December, 31st 2012, 26 patients had identifiable CNS involvement confirmed by biopsy / presence of plasma cells in the cerebrospinal fluid (CSF) and/or identification of intraparenchymal or meningeal involvement by imaging (MRI/CT). Patients were risk stratified by mSMART (Mayo Stratification for Myeloma And Risk-adapted Therapy) criteria. Overall survival (OS) from diagnosis and the time of CNS involvement was calculated using the Kaplan-Meier method.
Myelomatous CNS involvement occurred in 26 (0.6%) patients with MM of whom 3 were newly diagnosed. The median time to detection of CNS involvement was 24 months (range: 0-125) from diagnosis of MM. Median age at CNS myeloma diagnosis was 58 years (range 37-80) and 73% were male. Abnormally high LDH was observed in 11 out of 22 patients at the time of CNS involvement. Lumbar puncture was performed on 16 patients, 13 (81%) of whom had plasma cells in the CSF detected by cytology/flow-cytometry. Two patients, without evidence of plasma cells, had abnormally high CSF protein and 1 had normal CSF analysis. Of the 25 patients who underwent MRI, 16 (64%) had at least one of the following significant abnormalities; intraparenchymal disease (37%), leptomeningeal enhancement (68%) or direct extension of MM (31%). The neurological symptoms at or after diagnosis of CNS myeloma included headache (38%), cranial nerve palsy (38%), visual disturbance (38%), gait disturbance (35%), paresthesias (35%), limb weakness (31%), confusion (30%), nausea/vomiting (15%), dysarthria (12%), seizures (8%) and urinary incontinence (4%). Fluorescent in-situ hybridization (FISH n=7), cytogenetics (n=8) and/or plasma cell labeling index (PCLI n=12) were available in 18 patients prior to the diagnosis of CNS disease. Ten (56%) out of those 18 patients had high-risk features at least by one criterion. At the time of CNS involvement, six additional patients demonstrated high risk features [5 by PCLI (≥ 3%) and 1 by FISH]. Overall, 16 out of 26 (62%) patients were classified as high risk by mSMART criteria prior to or at the time of CNS involvement. Four (27%) out of 15 had a deletion p53 or monosomy 17 chromosomal abnormality. Median OS was 42 (95% CI, 19-55) months from the diagnosis of MM and 3 months (95% CI: 1-7.9) from the time of CNS involvement (Figure). OS of patients with high risk features was significantly worse (27 months) compared to standard risk disease (67 months, p=0.02) from diagnosis of MM. Eighteen patients received radiation therapy for CNS myeloma. Five of those patients also received intrathecal (MTX and ARA-C) therapy. One patient received intrathecal and systemic chemotherapy. Four patients did not receive any treatment. Novel agents, including bortezomib (23%), thalidomide (15%), and pomalidomide (4%) were administered to the patients post diagnosis of CNS disease. Six (23%) patients underwent autologous stem cell transplant post diagnosis of CNS disease with a median OS of 19 months (95% CI: 10-122 months) from the time of CNS involvement.
CNS involvement is a rare complication of MM that portends a poor survival outcome. It is likely that the rates in this study are an underestimate of the true incidence due the perceived futility of CNS directed therapy in this disease. Among those recognized, high-risk genetic and markers of increased proliferative activity, including deletion p53 / monosomy 17 and elevated PCLI (≥ 3%) appear to cluster in this cohort. Current therapeutic approaches are largely ineffective in managing this aggressive subset of myeloma patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal