Abstract
New therapies have resulted in improvements in myeloma survival, with increasing numbers of patients receiving treatment over several years. Despite this progress, the remitting and relapsing course of the disease continues to be associated with increases in patient morbidity and mortality due to skeletal related events (SREs), including fractures and spinal cord compression. Contemporary information on SRE frequency in myeloma patients at a population-based level is, however, sparse. The aim of this study was to evaluate the incidence of SREs and associated inpatient (I/P) reimbursement costs for myeloma patients.
Myeloma patients newly diagnosed between 2004-9 were identified from a UK specialist population-based study (the Haematological Malignancy Research Network – www.hmrn.org) and followed-up until April, 2011. Information on diagnosis, treatment (first and subsequent lines) and response was abstracted from medical records and all subjects were linked to Hospital Episodes Statistics (HES), a national database containing details of all hospital admissions in England. In our analyses, SREs within HES were identified by diagnosis and procedure codes using International Classification of Diseases (ICD-10) and Operating Procedure Code Set (OPCS-4), respectively. Associated reimbursements were estimated using Healthcare Resource Group (HRG codes); this was done for both SRE related events and the total inpatient treatment pathway.
Of the 1,112 patients newly diagnosed (median age 72.6 years, 57% males, incidence rate - 6.7 per 100,000), 72% received induction chemotherapy; the remainder received supportive care or radiotherapy only, or were asymptomatic and actively monitored. Overall, 32% of patients had an I/P episode related to an SRE; with 15% having non-vertebral fractures, 6% vertebral fractures, 6% spinal cord compression and 17% undergoing surgery to bone (Table 1).
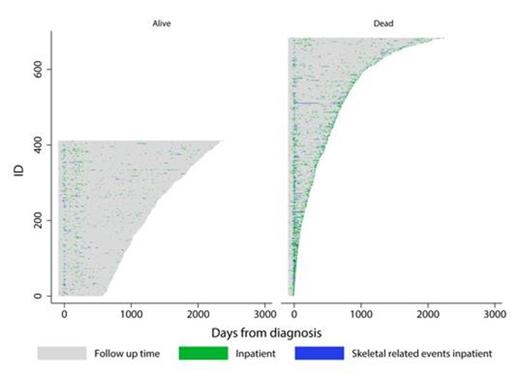
The Figure, which presents data by vital status, clearly shows that SREs occurred throughout the pathway. Median follow-up time was 3.8 years and each individual patient's pathway is illustrated by a single grey line, spanning 90 days pre-diagnosis through to death/end of follow-up. SRE I/P episodes are shown in blue and other I/Ps in green. Overall, the average number of bed days for each patient, for any reason, was 43.6, with a total reimbursement cost (excluding drug costs for myeloma) of pounds sterling (GBP) 13,930, equating to GBP 656/month. For myeloma patients with an SRE, the total number of SRE related bed days was 27.3, and total SRE related reimbursement costs were GBP 4,488.
Skeletal Related Events & Health Resource Utilisation 90 days Pre-Diagnosis to Death/April 2011: HMRN Myeloma Diagnoses 2004-9
| . | Number of patients . | Total Inpatient Days (days) Mean (sd) . | Total Cost GBP Mean (sd) 1 . |
|---|---|---|---|
| All patients | 1112 | 44 (42) | 13930 (14120) |
| SRE2 Episodes only | 356 | 27 (29) | 4488 (4840) |
| SRE type | |||
| Non-vertebral fracture | 170 | 26 (24) | 4802 (4765) |
| Vertebral fracture | 69 | 22 (21) | 2624 (2698) |
| Spinal cord compression | 62 | 28 (40) | 4109 (4041) |
| Surgery to bone | 193 | 17 (16) | 3243 (3349) |
| Admission timing | |||
| 90 days before diagnosis: | |||
| All inpatient admissions | 935 | 12 (17) | 2397 (2584) |
| SRE2 Episodes only | 134 | 21 (21) | 2701 (2617) |
| Diagnosis to end of first-line treatment: | |||
| All inpatient admissions | 660 | 20 (24) | 5343 (5620) |
| SRE2 Episodes only | 136 | 20 (24) | 2357 (3326) |
| Post first-line treatment : | |||
| All inpatient admissions | 674 | 28 (36) | 12538 (12895) |
| SRE2 Episodes only | 157 | 21 (24) | 4399 (4968) |
| . | Number of patients . | Total Inpatient Days (days) Mean (sd) . | Total Cost GBP Mean (sd) 1 . |
|---|---|---|---|
| All patients | 1112 | 44 (42) | 13930 (14120) |
| SRE2 Episodes only | 356 | 27 (29) | 4488 (4840) |
| SRE type | |||
| Non-vertebral fracture | 170 | 26 (24) | 4802 (4765) |
| Vertebral fracture | 69 | 22 (21) | 2624 (2698) |
| Spinal cord compression | 62 | 28 (40) | 4109 (4041) |
| Surgery to bone | 193 | 17 (16) | 3243 (3349) |
| Admission timing | |||
| 90 days before diagnosis: | |||
| All inpatient admissions | 935 | 12 (17) | 2397 (2584) |
| SRE2 Episodes only | 134 | 21 (21) | 2701 (2617) |
| Diagnosis to end of first-line treatment: | |||
| All inpatient admissions | 660 | 20 (24) | 5343 (5620) |
| SRE2 Episodes only | 136 | 20 (24) | 2357 (3326) |
| Post first-line treatment : | |||
| All inpatient admissions | 674 | 28 (36) | 12538 (12895) |
| SRE2 Episodes only | 157 | 21 (24) | 4399 (4968) |
1Inpatient costs using 2008-09 NHS Tariff, excludes drug costs for myeloma (GBP, 1pound sterling=$1.545, 07/08/2013); 2Skeletal-Related Event (SRE)
In our contemporary UK population-based dataset, around a third of myeloma patients experienced at least one SRE associated I/P episode at some point in their pathway, with such events being at least as common after diagnosis and first/subsequent treatment(s) as before. Clearly, in the era of novel myeloma therapies, SREs remain an important cause of morbidity, attracting significant inpatient health care costs.
Individual Patient Pathways Showing Inpatient Episodes
Ashcroft:Celgene: Research Funding. Jack:Roche /Genentech: Research Funding. Roman:Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal