Abstract
Multiple myeloma (MM) is a disease of the elderly and the median age at diagnosis is 65 to 68 years; MM is rarely diagnosed in patients ≤40 years of age. Reports on the characteristics of the disease and the outcome of patients ≤40 years of age are limited. Thus, we sought to identify patients ≤40 years of age who were treated for symptomatic myeloma and describe their characteristics and outcome in the era of novel agents. Among 1239 consecutive patients who started therapy for symptomatic MM within the Greek Myeloma Study Group centers, between January 2000 and December 2012, 49 patients (3.95%) were ≤40 years of age. We compared their characteristics and outcome to that of patients 41-65 years of age, who are usually eligible for autologous transplantation and to patients >65 years, who are usually treated without high dose therapy.
Most patients ≤40 years were males (67% vs. 55% of patients 41-65 and 52% of patients >65 years, p=0.069). Osteolytic bone disease at diagnosis was present in 81% (vs. 74% in each of the other two groups, p=0.553) and 65% had an ECOG performance status (PS) ≤1 (vs. 66% of patients 41-65 and 44% of patients >65 years, p<0.001). Anemia at diagnosis (Hb <10 gr/dl) was less frequent in patients ≤40 years than in older ones (29% vs. 44% in patients 41-65 and 47% in patients> 65 years, p=0.037), while low platelet counts (<130x109/l) were similar (10% vs. 13% and 12%, respectively, p=0.871). Severe renal dysfunction (eGFR <30 ml/min/1.73m2) was less common in younger patients (8% vs. 16% vs. 21%, p=0.025). Advanced disease stage (ISS-3) was present in 22% (vs. 32% and 42% for the other age groups, respectively) and most patients ≤40 years were rated as ISS-1 (55% vs. 29% vs. 20% for the other age groups; p<0.001). IgA MM was less common in patients ≤40 years (14% vs. 20% vs. 27% of patients 41-65 and> 65 years) and IgD MM was more common (6% vs. 3% vs. 2%, respectively; p=0.003). Other features of advanced disease such as LDH ≥300 IU/L were similar although bone marrow infiltration was less extensive in patients ≤40 years (52% had plasma cell infiltration <40% vs. 29% and 35% of patients of the other age groups, p=0.002).
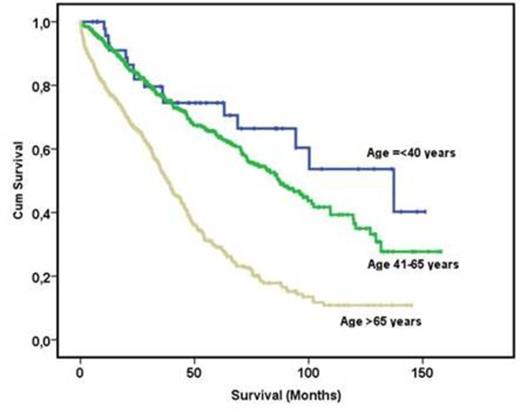
There were significant differences in the type of primary therapy among age groups: most patients ≤40 years received primary therapy with novel agents (47% bortezomib-based and 10% IMiD-based regimens), while patients in the other age groups received less often bortezomib at first line (38% of patients 41-65 years and 10% of patients >65 years received bortezomib but 17% and 47%, respectively, received primary therapy with IMiDs; p<0.001). Response to primary therapy was achieved in 75.5% vs. 76% vs. 69% of patients ≤40 years, 41-65 and <65 years respectively, but the quality of response was better in the younger patient group (sCR/CR in 33% vs. 19% vs. 11% and ≥ VGPR in 43% vs. 36% vs. 24% in the three age groups respectively, p<0.001). The calculated median survival for patients ≤40 years was 11.5 years (95% CI 7-16 years) vs. 7 years (95% CI 6-8.4 years) for patients 41-65 years (the difference was not significant p=0.162) and 3.2 years (95% CI 2.8-3.4 years) for patients >65 years (p<0.001 for comparison to the other two age groups). The survival curve indicates that only after 5 years there is a difference in the survival rate between patients ≤40 years and patients 41-65 years (74% vs. 64%). Compared to the survival of patients ≤40 years who started therapy between January 1990 and December 1999 (median survival 5 years) there has been a major improvement in the survival of younger patients (p<0.001). In order to adjust for differences in the characteristics of the disease between the three age groups (ECOG PS, ISS stage, anemia, renal dysfunction, IgA type) we performed a multivariate analysis in which the difference in the risk of death for patients ≤40 years vs. those 41-65 years was not significant (HR: 1.3, 95% CI 0.76-2.22, p=0.335); however, further follow up is needed in order to see a survival difference between these two groups of patients under the age of 65.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal