Abstract
Blood transfusions are given for acute and chronic illness including cardiothoracic surgery, acute stabilization, and chronic transfusion therapy (CTT) in patients with thalassemia and sickle cell disease (SCD). Increased age of stored red blood cells and the associated storage lesion has been implicated in poor cardiovascular outcomes, increased length of ICU stay, multiorgan failure and increased use of inotropes after cardiac surgery. Red cell aging, during storage, is thought to alter the metabolic profile of the red cell in a manner that causes decreased nitric oxide bioavailability. Aged red cells demonstrate vasoinhibitory activity of aortic ring preparations. S-nitrosohemoglobin is decreased in stored blood but when replete, tissue oxygen delivery and renal damage were ameliorated in an animal blood loss model. We aimed to determine whether the age of the stored blood relates to vascular function in-vivo, using a population of chronically transfused patients with SCD.
We did prospective study to examine transfusion effects on vascular function, in which we enrolled 26 patients with SCD on CTT and tested flow mediated dilation (FMD) of the brachial artery, cardiac output and blood viscosity changes with transfusion. We measured both oxygenated and deoxygenated whole blood viscosity at shear rates from 1s-1 to 1000s-1 at native hematocrit using a Rheolog viscometer (Rheologics Co). We also obtained pre and post transfusion measures of cardiac output, flow mediated dilation of the brachial artery, blood counts, chemistry panels, markers of inflammation and hemolysis.
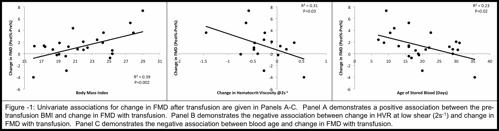
14 females and 12 males were enrolled. The ages and reasons for starting transfusions were similar for male and female patients. As expected, transfusion resulted in significant increases of hemoglobin and hematocrit (hct) with concomitant decrease of hemoglobin S% (HbS%) and reticulocyte count. Male patients had a significantly higher HbS%, reticulocyte count, plasma free hemoglobin and platelet count compared to females. Viscosity increased significantly across all shear rates with transfusion and with deoxygenation. There was no sex difference in viscosity. FMD was significantly improved following transfusion with an average increase of 1.4% (P=0.01). By univariate analysis, elevated body mass index (BMI), small change in hematocrit to viscosity ratio (HVR) at 2s-1 (low shear), and the lower age of the stored blood were significantly associated with improved FMD. By multivariate analysis, using only two variables at a time due to small sample size, elevated BMI was the best predictor of improved FMD. (Figure 1) There was a confounding effect between the age of the blood and BMI in our study; there was a negative correlation between age of the blood given and BMI, whereby smaller patients received older blood in our cohort.(R2 0.20, P=0.03). BMI did not correlate with pre-transfusion FMD.
Most patients with SCD on CTT had improved FMD following transfusion and given the dependence of FMD on shear stress, changes in rheologic factors such as viscosity and hematocrit would be expected to cause significant changes in FMD. The increase in hct, and viscosity and the decrease in HbS% did not correlate with improvement in FMD. Decrease in low shear HVR did correlate with improved FMD, however, FMD is thought to correlate with higher shear rates, whereas the HVR at low shear rate would be found in the venous system. This could provide a link between endothelial function and the low shear venous system, particularly due to its FMD correlation with “deoxygenated” HVR. BMI and age of the stored red cells correlated whereby our smaller patients received older blood resulting in confounding between these variables. Despite the confounding effect, when blood age was locked in the model, BMI still exerts an independent effect on FMD. Whether the effect of BMI is chronic or acute could not be determined in our study; however, nutritional factors, adipose tissue and hormones might play a role in the set point of FMD via eNOS expression in the endothelium. Older blood age was associated with worsening FMD, which is consistent with decreased nitric oxide bioavailability as a piece of the red cell storage lesion puzzle. Future studies should attempt to control for BMI and blood age to minimize confounding effects.
Coates:Novartis Inc.: Honoraria, Speakers Bureau; Apopharma: Honoraria, Speakers Bureau; Shire: Speakers Bureau. Wood:Shire: Consultancy, Research Funding; Apopharma: Honoraria, Patents & Royalties; Novartis: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal