Abstract

The immune-editing effect of myeloid leukemia has recently been reported in several studies. We previously demonstrated that the K562 leukemia-derived cell line suppresses T cell proliferation, which suggests that myeloid leukemia may function in a similar way to myeloid derived suppressor cells (MDSC). While the mechanism of suppression in leukemia is not fully understood, recent murine and human studies suggest that the STAT3 and arginase pathways play a key role in the immunosuppressive function of MDSC. We hypothesized that myeloid leukemia utilizes the MDSC STAT3 and arginase pathway to evade immune control, and block anti-leukemic immune responses.
To evaluate the suppressive capacity of myeloid leukemia on T cell proliferation, we isolated CD34+ blasts and myeloid derived suppressor cells (MDSC: CD11b+CD14+) from blood of primary leukemia samples by FACS sorting (n=5). These cells were co-cultured with CFSE-labeled CD4+ T cells (n=9), previously isolated from healthy donor PBMCs using an automated cell separator (RoboSep). After stimulating with CD3/CD28 Dynabeads (Invitrogen, New York, USA) for 72 hours, proliferation was measured by CFSE dilution of the viable cell population. In three myeloid leukemias studied, CD4+ T cell proliferation was significantly suppressed in the presence of primary CD34 blasts and MDSC cells (p<0.001). Interestingly, CD34 blasts demonstrated a greater suppressive effect on T cells compared to MDSC cells for these samples (not statistically significant p=0.61). Next we repeated the proliferation assay using five leukemia cell lines: THP-1 and AML1 (derived from AML), K562 and CML1 (derived from CML), and the Daudi lymphoid-derived leukemia cell line. After staining with cell tracer dye and irradiating 100Gy, the cells were co-incubated with CFSE-labeled CD4+ T cells from healthy volunteers (n=6). We found that CD4+ T cell proliferation in the presence of the myeloid leukemia cell lines was significantly suppressed (mean proliferation 5.7±0.9% to 26.1±10.7%: p<0.0001 to 0.05) compared to lymphoid cell lines (mean proliferation 76.3±8.2%: p>0.05), consistent with the results obtained with the primary leukemia samples.
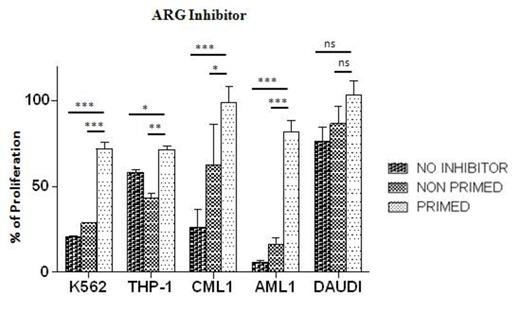
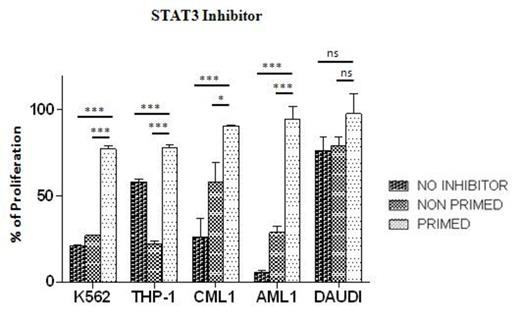
To evaluate the impact of STAT3 and arginase on the immunosuppressive function of myeloid leukemia, the five cell lines were primed overnight with either arginase inhibitor (N(ω)-Hydroxy-nor-L-arginine; EMD Biosciences, Inc., California, USA) or two STAT3 inhibitors (STAT3 Inhibitor VI or Cucurbitacin I; EMD Millipore, Massachusetts, USA). Then, CD4+ T cells from healthy donors (n=3) were cultured with either (1) leukemia without any inhibitor (2) leukemia in the presence of inhibitor (3) leukemia primed with inhibitor. Priming leukemia with arginase inhibitor and STAT3 inhibitors almost completely abrogated their suppressive effect of T cell proliferation (p<0.001).
We conclude that myeloid leukemia, like MDSC, directly immunosuppresses T cells, through STAT-3 and arginase. This finding may underlie the immune-editing of T cells by myeloid leukemia. Our results suggest that STAT3 inhibitors could be used to augment leukemia-targeted immunotherapy. Further investigation of T cell biology within the leukemia microenvironment is needed to further define immune editing mechanisms in myeloid leukemia.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal