Abstract
There is little evidence to support the efficacy of dosage exceeding conventional high dose chemotherapy (HDC), referred to as super-HDC (SHDC) for Acute Leukemia (AL). However our hospital has been successfully conducting an original SHDC and has realized the highest complete remission rate and 10 years event free survival ratio for all generations with no selection bias. For example, de novo AML except M3 results are 91%, 59% for under 70 years old and 75%, 32% for over 70 years old respectively (51st ASH #1052, until 2010). The treatment of complications is the key to SHDC success, with fungal infection one of the major complications. With our unique preemptive approach, we have successfully eliminated fungal mortalities on all AML patients with no selection bias (53st ASH #1544). In this group using ITCZ as prophylaxis, pulmonary invasive aspergillosis (PIA) morbidity rate was still high, so we had to switch from ITCZ to VRCZ. Thus we theorized that VRCZ is more effective as prophylaxis. As there is little supporting data, we scheduled this prospective randomized study commencing 2011/4/23. This is the interim analysis of the first 100 of 200 patients as of 2012/9/26.
All AL patients without a history of PIA who received induction chemotherapy were included. The patient number was dictated by our previous GM positive rate (30%). Either VRCZ or ITCZ were randomly assigned at admission and commenced from day 5. VRCZ as tablet at 400-600 mg/day, ITCZ as capsule at 150-200 mg/day. The primary end point is PIA morbidity rate and the secondary end points are all cause mortality, fungal infection mortality, non-PIA fungal infection, non-assigned antifungal drug use and PIA treatment efficiency using GM.
This study is unique as diagnostic and treatment strategies are completely unified for all. We conducted GM twice a week with CT at the time of admission and weekly. Additional CT was conducted within 24 hours when pyrexia of ≥38.0°C occurred, without improvement CT was repeated every 3 days. Our concept is original preemptive therapy, we assumed PIA when GM ≥0.5, and VRCZ was automatically started. Combination therapy using Micafungin (MCFG) was routinely conducted when PIA continued to worsen. Per contra we assumed candida infection, and conducted MCFG treatment, when the results met our original twice weekly surveillance culture and ß-D glucan criteria.
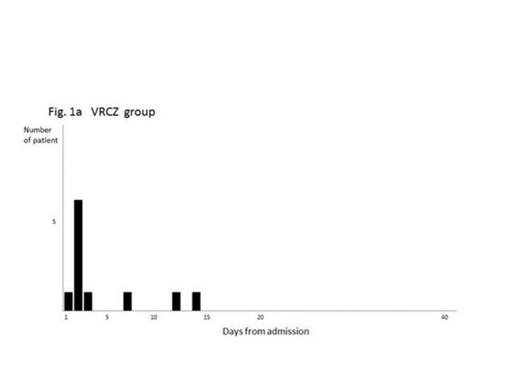
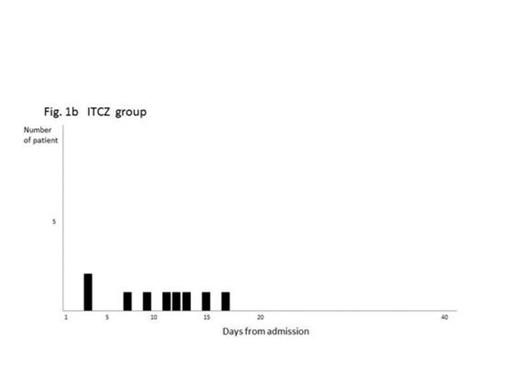
All cause mortality rate was identical, 6%. In VRCZ group (gp) AL progression was the sole cause. In addition to AL progression, 1 fungal infection caused by Cunninghamella was proved in ITCZ gp. Non-PIA fungal infections were only seen in ITCZ gp, Trichosporonemia, Candidemia or Cunninghamella pneumoniae were proved in three different patients. For non-assigned antifungal drug use, MCFG was comparable. VRCZ 60% (30/50), 17days (2-62), versus (vs) ITCZ 64% (32/50), 15 days (2-154). L-AmB was prescribed less in VRCZ gp (4% vs 8%) and VRCZ was prescribed to 18 ITCZ gp patients. The ITCZ gp required more drugs. Regarding PIA treatment efficacy using GM, was evaluated by max GM, number of days at max GM and final GM. All data median plus range. VRCZ was superior in every aspect, with 0.8 (0.5-3.1), 15 (9-53), 0.2 (0.1-1.5) results vs 2.35 (0.5-5.1), 28 (2-44), 0.65 (0.2-1.3) for ITCZ.
Using our peerless fugal strategies, satisfactory results were realized for both gp. PIA onset was found to be much earlier, so morbidity appears comparable. However, VRCZ superior results including better PIA control appears to be achieved due to early PIA onset, and supports VRCZ prophylactic use.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal