Abstract
Chuvash polycythemia (CP) is a rare congenital polycythemia caused by mutations in the VHL gene. Patients with CP present with erythrocytosis and are at high risk for thrombosis. Accordingly, CP patients have a significantly reduced lifespan. Currently, there are no proven therapies for CP. Studies demonstrating a potential benefit from phlebotomy or myelosuppressive agents have been lacking.
CP exhibits features of both secondary and primary polycythemia. The former has been attributed to dysfunction of the mutant VHL protein leading to upregulation of HIFa under normoxic conditions, thereby resulting in increased erythropoietin (Epo) production. The latter is manifested by hypersensitivity of CP erythryoid progenitors to Epo in vitro, but the mechanism for this finding has not been fully explained.
Recently, the VHL protein was shown to target phosphorylated JAK2 (pJAK2) for ubiquitin-mediated degradation. CP-associated VHL mutants were unable to degrade pJAK2, thereby leading to hyperactivation of downstream STAT signaling. In a CP mouse model, treatment with a JAK2 inhibitor led to normalization of hematocrit and reduction in splenomegaly. These findings provide a strong rationale for JAK2 inhibition as a therapeutic modality for CP. We now report preliminary data from two CP patients treated with the JAK inhibitor ruxolitinib.
Baseline and on-treatment characteristics for the two patients are summarized in Table 1 . Both patients were confirmed to be homozygous for the VHL R200W mutation. CP-01 first presented with erythrocytosis at 18 months. He was treated with intermittent phlebotomies and underwent a splenectomy at age 10. The patient had multiple thrombotic complications, including a deep vein thrombosis, pulmonary embolism, and portal vein thrombosis. He suffered from recurrent episodes of severe abdominal pain presumed to be related to his history of intra-abdominal thrombosis. The patient had a hemoglobin as high as 22.0 g/dL, and required four phlebotomies in a span of four weeks to achieve a hematocrit of 45.2% prior to initiating ruxolitinib.
CP-01 was initiated on ruxolitinib at a starting dose of 10 mg orally twice daily and titrated up to the current dose of 20 mg twice daily. As of the most recent follow-up at 12 weeks, the patient has not required any phlebotomies since starting ruxolitinib and has not had any new episodes of abdominal pain.
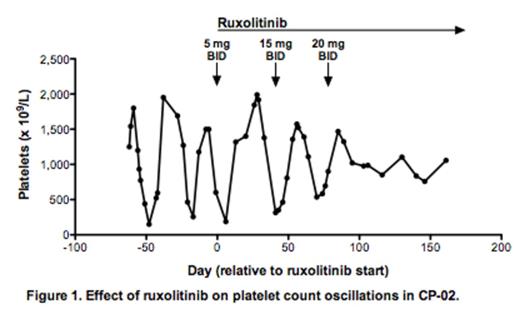
CP-02 was initially found to have erythrocytosis at the age of three. He was treated with intermittent phlebotomies but developed multiple thrombotic complications, including mesenteric vein thrombosis as well as a myocardial infarction at the age of 27. He also suffered from severe back pain presumed to be related to bone marrow expansion. The patient exhibited oscillations in his platelet count that were exacerbated after he underwent a splenectomy (platelet counts ranging between 7 x 109/L and 1900 x 109/L on a ∼30 day cycle). Periods of extreme thrombocytosis were associated with severe headaches requiring plateletpheresis.
To our knowledge, these two cases represent the first CP patients treated with a targeted inhibitor of JAK2. Both patients have experienced hematologic and symptomatic improvement, with no significant safety issues to date. These preliminary observations validate pre-clinical studies suggesting a role for JAK2 inhibition in CP. Correlative studies examining endogenous erythroid colony formation, JAK-STAT signaling, and inflammatory cytokine levels are ongoing.
Oh:Incyte: Consultancy, Research Funding, Speakers Bureau. Off Label Use: Ruxolitinib for Chuvash polycythemia.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal