Abstract
Mantle cell lymphoma (MCL) is an aggressive B-cell non-Hodgkin lymphoma (NHL) which is characterized by the t(11;14)(q13;q32) translocation leading to overexpression of cyclin D1 that consists of around 3% of NHL. Most cases are diagnosed at advanced stage and despite the progress in the treatment, the prognosis remains poor. Appropriate prognostification of the disease is essential to consider risk stratified treatment to improve the outcome. Although MCL international prognostic index (MIPI) has been reported as the specific prognostic index of MCL, most of the patients included in the study received chemotherapy without rituximab. Validation of MIPI in rituximab era has been done by several studies but the result remains controversial.
To evaluate the treatment outcome and prognostic factors of MCL in Japan, we conducted a multicenter retrospective study. Medical records of 633 patients with MCL newly diagnosed and treated from 63 hospitals between 1992 and 2012 were reviewed and analyzed. Pretreatment characteristics and treatment regimens were evaluated for their association with overall survival (OS) and progression free survival (PFS) by hazard ratio (HR). Since the patients received various chemotherapy regimens, treatment were adjusted to analyze prognostic factors.
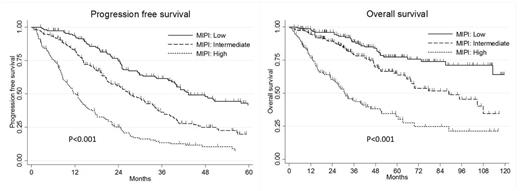
The median age of patients was 66 years old (range 22-92). Ninety percent of the patients were in stage III/IV, 70% had bone marrow involvement and 12% had poor performance status. According to the simplified MIPI (s-MIPI), 191 patients (32%) were classified as low risk, 233 patients (39%) were classified as intermediate risk and 169 patients (29%) were classified as high risk. Among the patients, 504 patients (82%) received rituximab containing chemotherapy, 55% received CHOP-like regimen, 32% received high-dose Ara-C containing regimen (HDAC) and 17% received autologous stem cell transplantation (ASCT) at the first-line treatment. With a median follow up duration of 43.4 months, overall 3-years PFS and OS was 36% and 73%, respectively. By limiting the analysis to the patients who received rituximab at the first-line treatment, s-MIPI was still a valid prognostic index for both PFS and OS even in the rituximab era (Figure), with 3-years PFS for low, intermediate and high MIPI of 62%, 36% and 14%, respectively. Multivariate analysis by Cox model revealed that Hb<12mg/L (HR: 1.4 [1.0-2.0]), beta 2-microglobulin≥4.0 µg/L (HR: 2.4 [1.4-4.0]) and total protein<6.0g/dl (HR: 1.8 [1.2-2.9]) were significantly associated with shorter OS independent to s-MIPI. With the stratification by s-MIPI at the analysis, treatment regimen was significantly associated with the outcome in rituximab era that 3-years PFS for CHOP, CHOP+ASCT, HDAC, HDAC+ASCT of 21%, 54%, 52% and 76%, respectively. HDAC regimen was significantly associated with longer PFS than CHOP regimen (HR: 0.40 [0.31-0.52]). With focusing on ASCT, upfront-ASCT were associated with longer PFS both in CHOP (HR: 0.39 [0.19-0.81]) and HDAC regimen (HR: 0.66 [0.42-1.1]).
s-MIPI is a valid prognostic index even in the rituximab era. We also identified three prognostic factors independent to s-MIPI including anemia, high beta 2-microglobulin and low total protein. Upfront ASCT showed survival benefit both in CHOP and HDAC regimen.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal