Abstract
Clinical impact of chronic hepatitis B virus (HBV) and hepatitis C virus (HCV) infections is not well studied in a large series of patients with lymphoma undergoing autologous stem cell transplantation (ASCT). Retrospective analysis was performed to evaluate clinical outcomes of patients with lymphoma receiving ASCT with or without HBV and HCV infections.
Among 13218 adult patients registered in the Adult Lymphoma Working Group of the Japan Society for Hematopoietic Cell Transplantation (JSHCT) database, we selected patients who had the information on HBV and HCV infection status and received ASCT from 1989 to 2010. Patients diagnosed as Hodgkin lymphoma, mature or precursor T- and B-cell lymphoma were included. Histological diagnosis of natural killer (NK)-cell lymphoma and adult T-cell leukemia/lymphoma were excluded in this analysis. Patients who had human immunodeficiency virus (HIV) infection and history of previous transplantation were also excluded. Survival analysis was performed to compare patients positive for HBV and HCV with those negative for both. Prognostic indicator for survival was also investigated in patients positive for HBV and HCV.
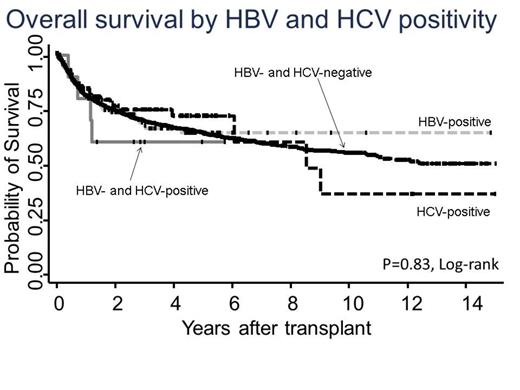
A total of 4641 patients with 2819 male were analyzed. The median age of all patients was 54 years (range: 16-81 years). The patient characteristics were summarized in Table 1. HBV and HCV infections were present in 162 (3.5%) and 104 (2.2%) patients, respectively. Ten patients (0.2%) had both HBV and HCV infections. Detailed data on anti-HBV antigen or antibody and genetic data were not available in the analysis. Patients with HBV and HCV infections were older and more diagnosed with advanced stage than those without infections. With a median follow-up of 2.8 years, the 2-year overall survival (OS) rate of all patients was 75% (95%CI: 73 to 76). Cumulative incidence of treatment-related mortality (TRM) at one year after ASCT was 5.8% (95%CI: 5.2 to 6.6). According to HBV and HCV positivity, the estimated 2-year overall survival (OS) rates were 74% (95%CI: 65 to 81), 77% (95%CI: 66 to 84), 60% (95%CI: 25 to 83) and 75% (95%CI: 73 to 76) in patients with HBV-positive, HCV-positive, both virus positive and negative patients, respectively. Cumulative incidence of TRM at one year was 11% (95%CI: 6.2 to 16) 6.6% (95%CI: 2.7 to 13) and 5.7 (95%CI: 5.0 to 6.4) in patients with HBV-positive, HCV-positive and both virus negative patients, respectively. In patients with or without HBV and HCV infections, there was no statistically significant difference in rates of OS (p=0.82, Figure 1) and TRM (p=0.63).
Overall survival according to the positivity of HBV and HCV in patients with lymphoma undergoing autotransplant
Overall survival according to the positivity of HBV and HCV in patients with lymphoma undergoing autotransplant
In multivariate analysis of patients infected with HBV, factors associated with shorter OS were male sex (HR: 3.1, 95%CI: 1.2 to 7.6), non-remission/relapse status at ASCT (HR: 2.7, 95%CI: 1.2 to 5.9) and ASCT before 2005 years (HR: 3.6, 95%CI: 1.6 to 8.4). ASCT before 2005 years was associated with higher TRM in patients with HBV infection (HR: 4.4, 95%CI: 1.5 to 13). In patients with HCV infection, multivariate analysis revealed that partial remission (HR: 3.5, 95%CI: 1.2 to 10.6), non-remission/relapse (HR: 5.3, 95%CI: 1.9 to 14.6) status at ASCT and age≥ 50 years at ASCT (HR: 7.0, 95%CI: 1.5 to 31.9) were significantly associated with shorter OS. Non-remission/relapse status at ASCT was associated with higher TRM in patients infected with HCV (HR: 4.4, 95%CI: 1.1 to 18.3). Difference in histology was an adverse factor for outcomes in the HBV- and HCV-negative groups, however, the factor could not be identified as adverse indicator in the HBV- and HCV-positive groups.
Prognosis of patients with HBV and HCV infections would be comparable to patients without those infections. Disease status at ASCT could be one of useful landmarks to predict outcomes in patients positive for HBV and HCV undergoing ASCT. After careful consideration, ASCT might be a feasible option for patients with HBV and HCV infections.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal