Abstract
Although diagnostic and treatment delays in solid tumors are known to negatively impact on outcomes, little is known with respect to hematological malignancies. Diffuse Large B-Cell Lymphoma may present with a wide array of symptoms, thus rendering initial diagnosis challenging and time consuming. We evaluated disease-specific, patient-related and socioeconomic factors leading to delays in DLBCL diagnosis and treatment and the respective impact on overall and progression-free survival. Methods A comprehensive clinical database of patients with a new diagnosis or new presentation of transformed DLBCL treated at our center between 2002 and 2010 was utilized. A total 278 patients were included. All patients received at least one cycle of Rituximab, Cyclophosphamide, Doxorubicin, Vincristine, and Prednisone (R-CHOP) immuno-chemotherapy. We defined various time intervals based on Cancer Care Ontario guidelines as follows: patient associated delay – time from symptoms onset to first known contact with a primary care physician (PCP); diagnostic delay – >6 weeks from first PCP contact to initial hematology consultation; and treatment delay – >4 weeks from first hematology consultation to chemotherapy initiation.
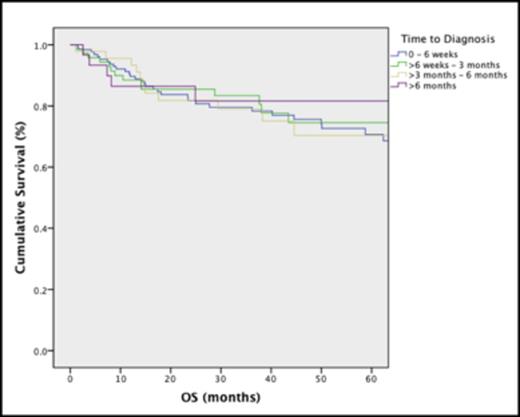
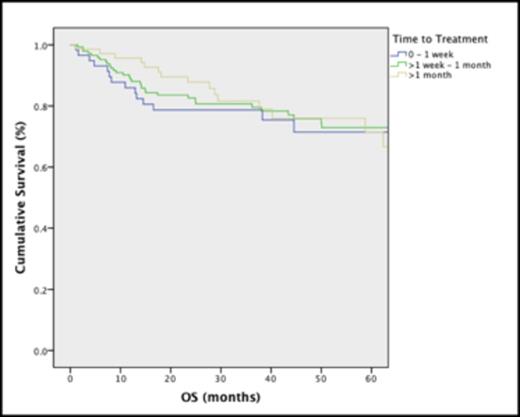
In the population studied (n=278), the median age was 63 and 46% were female. Patients waited a median of 4 weeks (IQR 2-13) before seeking medical attention. A further median of 8 weeks (IQR 4-17) was required for the PCP to diagnose DLBCL or at least to achieve enough clinical suspicion for referral to hematology. From initial hematology consult, a median of 3 weeks (IQR 1-4) elapsed until chemotherapy initiation. In univariate analyses, patients who lacked bone marrow involvement (p=.005), had lower IPI scores (p=.031), higher Charlson comorbidity index (p=.048) and who had initiation of treatment in the outpatient setting (vs. inpatient; p=.021), were more likely to experience diagnostic delays >6 weeks. In multivariable logistic regression analysis, bone marrow involvement (OR=0.41, p=.018), Charlson comorbidity index (OR=1.42, p=.017) and requirement for urgent inpatient chemotherapy administration (OR=0.40, p=.012) remained associated with diagnostic delays. With respect to treatment delays, in univariate analyses, patients who did not have a pathology diagnosis at the time of initial hematology consultation (p<.0001) and those with B symptoms (p=.039) were more likely to experience treatment delays >4 weeks. On multivariable analysis, lack of pathological diagnosis at the time of hematology referral was the only factor that remained associated with treatment delays (OR=8.25, p<0.001). No socioeconomic factors (low income, level of education, and cohabiting alone) predicted for either diagnostic or treatment delays. On Cox multivariable regression analyses, diagnostic (Fig 1) or treatment delays (Fig 2) did not impact on survival or progression-free survival; only IPI score and number of R-CHOP cycles significantly impacted overall survival (HR=1.82, p<.001; HR=0.70 p<.001) and progression-free survival (HR=1.56, p<.001; HR=0.82, p=.004).
Delays in DLBCL diagnosis of 6 weeks to over 6 months do not affect overall survival.
Delays in DLBCL diagnosis of 6 weeks to over 6 months do not affect overall survival.
Delays in DLBCL treatment of over 1 month do not affect overall survival.
Delays in DLBCL treatment of over 1 month do not affect overall survival.
Selected disease and patient-related factors may be associated with delays in management of DLBCL. However, unlike in solid tumor presentations, we can reassure patients that waiting a reasonable time frame to complete diagnostic and staging milestones should not affect their disease course, as long as appropriate chemotherapy dosing is administered.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal