Abstract
The role of bone marrow (BM) involvement as prognostic factor in untreated young patients with diffuse large B-cell lymphoma at poor prognosis is still a matter of debate. Recent data showed an adverse prognostic role of BM involvement in DLBCL including patients both at low and high IPI score (Sehn L et al, J Clin Oncol 2011). On this basis, FIL analyzed the impact of BM involvement in the prospective randomized phase III trial DLCL04 (Vitolo U et al, Blood, ASH annual Meeting 2012) that included only young patients at high-risk age-adjusted IPI (aa-IPI) score 2 or 3.
Inclusion criteria were: age 18-65; untreated DLBCL or follicular grade IIIb; aa-IPI score 2 or 3. Patients were stratified according to aa-IPI and randomized at diagnosis to receive: R-CHOP14 x 8 cycles; R-MegaCHOP14 (1200 mg/sqm Cyclophosphamide, 70 mg/sqm Doxorubicin, standard dose Vincristine and Prednisone) x 6; R-CHOP14 x 4 + R-HDC (Rituximab + High Dose Cytarabine + Mitoxantrone + Dexamethasone) followed by BEAM and ASCT; R-MegaCHOP14 x 4 + R-HDC + BEAM and ASCT. BM biopsy and aspirate were mandatory at diagnosis; at the end of treatment, BM assessment was mandatory only in case of positivity at baseline. BM involvement was defined as concordant if marrow was involved by large B-cell and discordant if involved by small B-cells. Flow cytometry, immunohistochemistry, and/or molecular studies were utilized to confirm a clonal B-cell population.
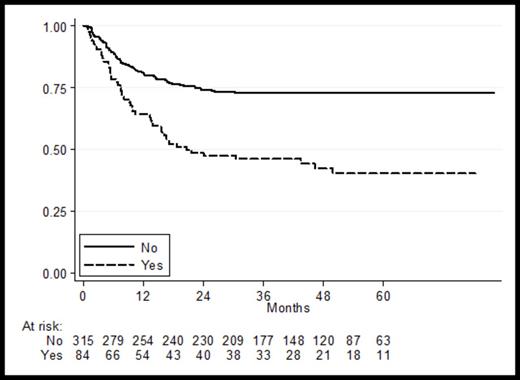
From June 2005 to September 2010, 399 patients were randomized to receive: 199 R-HDC+ASCT and 200 R-dose-dense chemotherapy without ASCT. All patients were evaluable for analysis. BM involvement was reported in 84 patients (21%): 39 (20%) in the R-HDC+ASCT group and 45 (22%) in the R-dose-dense chemotherapy group. Pattern of involvement was: concordant in 63 patients, discordant in 14 and not specified in 7 patients. Patients with BM involvement (BM positive: 84) compared to those without BM involvement (BM negative: 315) were significantly older (median age 53 years vs 47 years, p<.001) and at higher aa-IPI score (aa-IPI 3: 36% vs 24%, p .024); whereas other clinical characteristics were well balanced between the two groups (ECOG PS >1 43% vs 45%, bulky 25% vs 33%, extranodal sites > 1 26% vs 33%, LDH higher than normal value 93% vs 89%). With a median follow-up of 49 months, 3-year PFS for the whole series of 399 patients enrolled in the trial was: 67% (95% CI: 62-72). Three-year PFS was significantly worse in BM positive vs. BM negative: 46% (95% CI:35-56%) vs. 73% (95% CI:67-77%) p<.001 (Figure 1). In a Cox-model for PFS including type of treatment (ASCT vs no-ASCT, RCHOP vs R-MegaCHOP), age, gender, aa-IPI, performance status, histology and BM involvement, the adverse prognostic impact of BM involvement was maintained with an adjusted Hazard Risk (aHR) of 2.22 (95% CI:1.54-3.22, p<.001).Three-year OS rates in BM positive vs. BM negative were: 65% (95% CI:53-74%) vs. 83% (95% CI:78-87%) with an aHR 1.94 (95% CI:1.23-3.05; p=.004). The adverse prognostic impact of BM involvement on PFS was not affected by the type of treatment and the application of HDC+ASCT: 3-year PFS in BM positive patients treated with R-dose-dense chemotherapy 42% (vs. 69% BM negative) with an aHR of 2.19 (95% CI: 1.35-3.54, p<.001); 3-year PFS in BM positive patients treated with HDC+ASCT 51% (vs. 77% BM negative ) with an aHR of 2.27 (95% CI:1.30-3.97, p<.004). We further analyzed the prognostic impact of the pattern of BM involvement (concordant vs discordant). With the limits of small sample size of the discordant group, concordant BM involvement maintained an adverse prognostic impact on PFS whereas discordant involvement did not affect PFS: in a Cox-model assuming BM negative as reference, the risk of progression was significantly increased in the concordant involvement group with an aHR of 2.48 (95% CI: 1.68-3.67, p<.001) and not affected by discordant involvement (aHR 1.05; 95% CI:0.41-2.71, p=.916).
Bone marrow involvement, namely concordant pattern, is a strong adverse predictor of outcome in young patients with untreated DLBCL at poor prognosis treated with R-chemotherapy regardless of intensification with HDC+ASCT. New treatment approaches are needed for these high-risk patients at poor prognosis.
Vitolo:Roche: Speakers Bureau; Takeda: Speakers Bureau; Celgene: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal