The post thrombotic syndrome (PTS) is a frequent complication of deep vein thrombosis (DVT), occurring in 20-40% of DVT patients. Identifying risk factors for PTS may be useful to provide patients with reliable prognostic information and target prevention strategies. Inherited and acquired thrombophilias are well established risk factors for DVT. We hypothesized that these markers may also increase the risk of PTS.
To conduct a systematic review to assess: Among patients with DVT, are inherited or acquired thrombophilias associated with risk of PTS?
We conducted a search of the electronic databases PubMed, EMBASE, Scopus, and Web of Science for studies published from 1990-2013. Studies were considered eligible if they reported assessing any thrombophilia in adult DVT patients and its association with the development of PTS. Risk of bias was assessed using a modified Newcastle-Ottawa scale. Meta-analysis was performed by pooling odds ratios (OR) using the random effects model, when three or more studies were available.
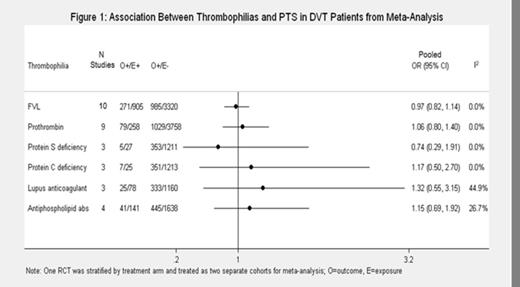
After removal of duplicates, 2376 records were screened and 84 full text articles were assessed for eligibility. Sixteen studies were included in our review: 13 studies assessed Factor V Leiden (FVL), 10 assessed prothrombin gene mutation, 5 studies assessed protein S and C deficiencies, 3 assessed antithrombin deficiency, 4 assessed factor VIII activity, and 6 studies assessed antiphospholipid antibodies (6 studies assessed Lupus Anticoagulant (LAC) and 1 assessed Anticardiolipin Antibody). None of the meta-analyses performed identified any inherited or acquired thrombophilia to be predictive of PTS (Figure 1). We were unable to pool studies reporting the association between Factor VIII and PTS because of clinical heterogeneity, however, descriptively, the predictive value of FVIII for PTS seems to be limited.
We conducted subgroup analyses stratifying studies by patient characteristics (Table 1). Both FVL and prothrombin mutations appeared to be protective for PTS among studies including patients with both first and recurrent DVT, and studies where >50% of patients had an unprovoked DVT. Our pooled estimate for the effect of antiphospholipid antibodies is largely based on studies that measured LAC while on anticoagulant treatment, hence may be an underestimate. However, the confidence intervals for the estimates overlapped the null for all of these subgroups.
Subgroup analyses
| Subgroup . | N studies meta-analyzed . | PTS/Positive Thrombophilia . | PTS/No Thrombophilia . | I2 . | Pooled OR (95% CI) . |
|---|---|---|---|---|---|
| FVL | |||||
| Overall | 101 | 271/905 | 985/3320 | 0.0% | 0.97 (0.82, 1.14) |
| First/recurrent DVT | 41 | 64/173 | 278/643 | 0.0% | 0.78 (0.54, 1.12) |
| First DVT | 6 | 207/732 | 707/2677 | 0.0% | 1.03 (0.85, 1.24) |
| ≤50% unprovoked DVT2 | 51 | 157/535 | 665/2312 | 0.0% | 1.04 (0.84, 1.29) |
| >50% unprovoked DVT | 4 | 89/262 | 253/692 | 19.9% | 0.78 (0.54, 1.13) |
| Prothombin mutation | |||||
| Overall | 91 | 79/258 | 1029/3758 | 0.0% | 1.06 (0.80, 1.40) |
| First/recurrent DVT | 31 | 10/39 | 247/574 | 0.0% | 0.46 (0.22, 0.97) |
| First DVT | 6 | 69/219 | 845/3184 | 0.0% | 1.22 (0.90, 1.64) |
| ≤50% unprovoked DVT2 | 41 | 49/155 | 688/2490 | 0.0% | 1.23 (0.86, 1.75) |
| >50% unprovoked DVT | 4 | 25/79 | 317/875 | 21.7% | 0.80 (0.44, 1.44) |
| Any Antiphospholipid antibodies | |||||
| Overall | 41 | 41/141 | 445/1638 | 26.7% | 1.15 (0.69, 1.92) |
| On anticoagulants or unknown | 3 | 36/134 | 383/1465 | 36.4% | 1.05 (0.63, 1.77) |
| Not on anticoagulants | 11 | 5/7 | 62/173 | 0.0% | 3.27 (0.53, 20.02) |
| Subgroup . | N studies meta-analyzed . | PTS/Positive Thrombophilia . | PTS/No Thrombophilia . | I2 . | Pooled OR (95% CI) . |
|---|---|---|---|---|---|
| FVL | |||||
| Overall | 101 | 271/905 | 985/3320 | 0.0% | 0.97 (0.82, 1.14) |
| First/recurrent DVT | 41 | 64/173 | 278/643 | 0.0% | 0.78 (0.54, 1.12) |
| First DVT | 6 | 207/732 | 707/2677 | 0.0% | 1.03 (0.85, 1.24) |
| ≤50% unprovoked DVT2 | 51 | 157/535 | 665/2312 | 0.0% | 1.04 (0.84, 1.29) |
| >50% unprovoked DVT | 4 | 89/262 | 253/692 | 19.9% | 0.78 (0.54, 1.13) |
| Prothombin mutation | |||||
| Overall | 91 | 79/258 | 1029/3758 | 0.0% | 1.06 (0.80, 1.40) |
| First/recurrent DVT | 31 | 10/39 | 247/574 | 0.0% | 0.46 (0.22, 0.97) |
| First DVT | 6 | 69/219 | 845/3184 | 0.0% | 1.22 (0.90, 1.64) |
| ≤50% unprovoked DVT2 | 41 | 49/155 | 688/2490 | 0.0% | 1.23 (0.86, 1.75) |
| >50% unprovoked DVT | 4 | 25/79 | 317/875 | 21.7% | 0.80 (0.44, 1.44) |
| Any Antiphospholipid antibodies | |||||
| Overall | 41 | 41/141 | 445/1638 | 26.7% | 1.15 (0.69, 1.92) |
| On anticoagulants or unknown | 3 | 36/134 | 383/1465 | 36.4% | 1.05 (0.63, 1.77) |
| Not on anticoagulants | 11 | 5/7 | 62/173 | 0.0% | 3.27 (0.53, 20.02) |
Notes: 1) One clinical trial stratified by treatment arm, 2) One study (Schulman 2006) not included
A sensitivity analysis was conducted to restrict to studies that used a more rigorous definition of PTS (using only the Villalta scale). FVL was associated with an OR 0.88 (6 studies; 95% CI: 0.66, 1.18) and prothrombin mutation with an OR 0.91 (6 studies; 95% CI: 0.55, 1.49). Hence, FVL appeared protective when we restricted to higher quality studies.
Our meta-analysis did not demonstrate a significant association between any of the thrombophilias assessed and the risk of PTS in DVT patients, however, we cannot rule out a mild protective effect of FVL and prothrombin mutation in certain subgroups. As the pathophysiology of PTS involves the complex interplay of persistent venous obstruction, valvular incompetence and inflammation, other biomarkers may be more predictive of the patient’s risk of PTS.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal