Abstract
As volume-based radiotherapy planning has become a more standard part of combined modality therapy for lymphomas, dose-volume based constraints for organs-at-risk are needed for treatment planning. Conformal techniques such as intensity modulated radiation therapy and proton radiotherapy may achieve lower doses to certain organs like the heart, but may result in higher doses to other tissues like the lungs and breasts. We sought to define the dosimetric risk factors that are associated with development of radiation pneumonitis (RP).
This is a single-institution retrospective analysis of patients with thoracic lymphomas treated with combined modality therapy between 1999 and 2013 who had at least 4 months of follow-up after radiotherapy. Univariate analyses (UVA) were performed using Fisher exact and Wilcoxon rank-sum tests.
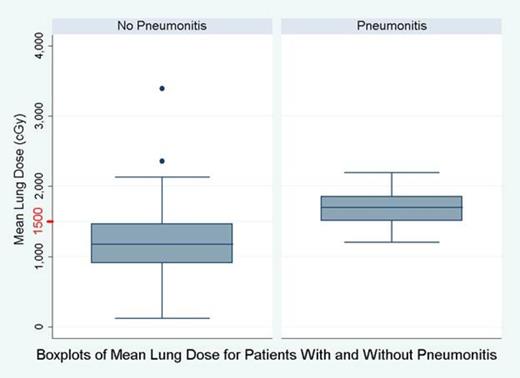
Of the 89 patients analyzed, 13 (14.6%) were diagnosed with RP (at least Grade 1, Common Toxicity Criteria v4.0). Patients were predominantly female (62%) and never smoked (67%). Diagnoses were grouped as Hodgkin lymphoma (62.9%) or non-Hodgkin lymphoma (37.1%), and 18.5% were also treated with autologous stem cell transplants. UVA showed that RP was more commonly associated with a diagnosis of non-Hodgkin lymphoma (38%) than Hodgkin lymphoma (8%), despite exposure to bleomycin in the majority of patients with Hodgkin lymphoma. Higher lung doses were significantly associated with RP using multiple lung dose-volume parameters: mean lung dose (12.3 vs. 16.7 Gy, p=0.002), volume of lung receiving 20 Gy (27.3% vs. 39.1%, p=0.0009), and volume of lung receiving 5 Gy (51% vs. 66.8%, p=0.004). The majority (67%) of patients who developed RP had mean lung doses of over 15 Gy, whereas only 24% of those who did not develop RP had mean lung doses above 15 Gy, see Figure. Heart dosimetric parameters were also significantly associated with RP, including mean heart dose (13.3 vs. 21.5 Gy, p=0.004), volume of heart receiving 20 Gy (25.4% vs. 48.3%, p=0.003), and volume of heart receiving 5 Gy (57.6% vs. 81.1%, p=0.04). There were not enough events to determine if heart and lung parameters were independently associated with RP, but they were strongly correlated (R=0.75).
Gender, smoking history, and autologous transplant were not significantly associated with RP. None of the 13 patients treated with proton radiotherapy developed RP. In general, patients treated with proton radiotherapy had lower mean heart doses (9.4 vs. 15.4 Gy) and mean lung doses (9.6 Gy vs. 13.5 Gy).
Higher doses to lung and heart are associated with increased risk of RP, and doses to these critical structures should be considered carefully during volume-based consolidative radiotherapy using advanced techniques.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal