Abstract
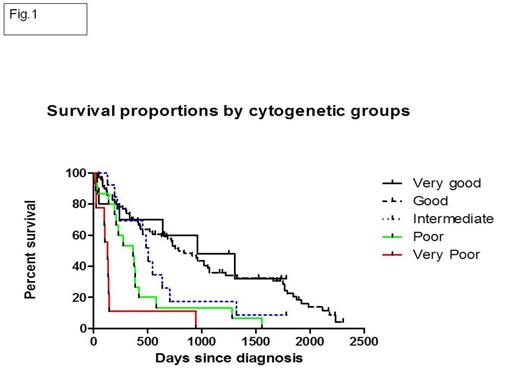
MDS encompasses a heterogeneous group of clonal marrow disorders resulting in various degree of ineffective hematopoiesis and risk of Acute Myelogenous (AML) transformation. Intuitively, the original IPSS (4-categories) lacked predictive power to dissect subgroups with more aggressive biological behavior suitable for MDS disease modifying strategies. The new coalesced R-IPPS discriminates biological subgroups and enhances predictive power based on redefined cytogenetic [5-categories-very good: -Y, del(11q); Good: e.g., normal karyotype, del(5q), del (20q); intermediate: e.g., +8,+19, del(7q); poor: e.g., -7 inv 3/del(3q), complex 3 abnormalities (abn); very poor: complex > 3 abn], depth of cytopenias and revised blast count subcategories at disease initiation, therefore allows more precise risk adapted intervention. Here, we aimed at validating the impact of cytogenetic subcategories on survival and initiated exploration of applicability of R-IPSS in our cohort of veterans diagnosed with MDS. This strategy allowed gaining insight into intrinsic disease characteristics and survival of our population.
From 2000-2012, 124 patients (pts) with confirmed diagnosis MDS were identified from the Michael E. Medical Center Cancer Registry. Long rank test was used to compare median Overall Survival (OS) in all generated cytogenetic and R-IPSS subgroups. Given the known effect of patient age on survival, all scored pts had survival age- adjusted using previously described formula (Greenberg. Blood. 2012).
Among pts studied, median age was 72 years (range, 53-91). With a median survival for the all cohort of MDS pts of 17.6 months (mo), the 3-years overall survival (OS) was 55%. In our cohort, cytogenetic classification revealed discriminative parameter from variables contained in R-IPSS with OS for very good of 32 mo (N= 10 [9.4%]), good of 26.2 mo (N=64 [59.8 %]), intermediate of 16.8 mo (N=10 [12.8%]), poor of 12.1 mo (N=14 [16.7%]) and very poor of 4.2 mo (N=9 [7%]) (P=0.5; P=0.11; P= 0.13,P =0.08; P=0.02, respectively) (Fig.1). R-IPSS was calculated as reported. Median OS for patients in low, very low, intermediate, high and very high-risk categories were 34, 35.5, 14.5, 15, 7.8 mo, respectively (Fig.2). Age adjusted median survival estimation allowed more robust discrimination of survival with median survival of 35.5 months (mo) (P=0.8; HR=1), 18.2 mo (P=0.49; HR=1.9), 15 mo (P=0.008; HR=2.1) and 8.5mo (P=0.00; HR=4.1) for low, intermediate, high and very high-risk subgroups (Fig.3). No statistical significance difference in survival was observed between very low and low risk categories.
Our results validate the predictive value of the newly developed cytogenetic risk stratification groups contained in R-IPSS. For cytogenetic risks, clinical trends were observed across very low, low, intermediate and poor risk with significant different survival seen between poor and very poor cytogenetic groups. When taking in consideration all variables included in R-IPSS, a more precise discrimination of biological subgroups was observed after cohort age-adjustment. Larger pts samples are needed to refine difference in survival between very low and low categories.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal