Abstract
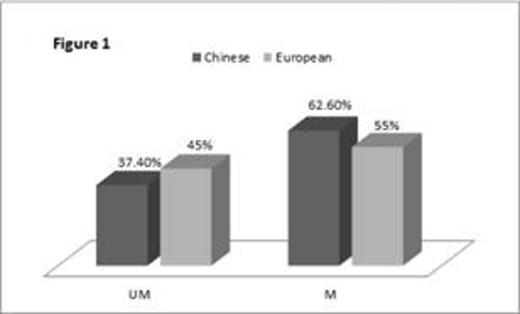
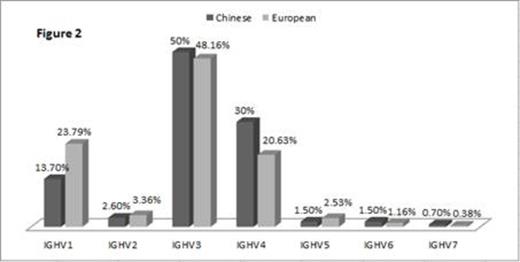
Different IGHV gene usage between Chinese and European CLL patients, with IGVH1 gene accounts for 23.79% of European CLL patients and for only 13.70% of Chinese CLL patients.
Different IGHV gene usage between Chinese and European CLL patients, with IGVH1 gene accounts for 23.79% of European CLL patients and for only 13.70% of Chinese CLL patients.
IGVH1-69 is the most prevalent IGHV gene among European CLL patients(12.81%), however, only 5.20% Chinese CLL patients use VH1-69. IGVH4-39 and IGVH4-59 are more often used in Chinese CLL patients (7.80% vs 3.73% and 5.60% vs 2.75%, respectively).
IGVH1-69 is the most prevalent IGHV gene among European CLL patients(12.81%), however, only 5.20% Chinese CLL patients use VH1-69. IGVH4-39 and IGVH4-59 are more often used in Chinese CLL patients (7.80% vs 3.73% and 5.60% vs 2.75%, respectively).
We further studied the distribution of stereotyped BCR in our cohort. Thirty-eight patients (14.07%) with stereotyped BCR that belonged to 21 subsets were identified, with 1 to 7 sequences contained each. Among them, subset 1 and subset 8 are the most common types with 6 and 7 cases respectively. Three new subsets were discovered (Table 1). Notably, only 1 case belonged to subset 2, the subset with largest group size in western world. Hence, we conclude that Chinese CLL patients show unique IGHV repertoire features compared to patients from western countries. While the mechanism within remains unknown, the discrepancy might due to antigenic difference in geographically remote areas.
Three new subsets of BCR stereotypy in Chinese CLL patients
| . | NO. . | IGHV . | IGHD . | IGHJ . | M/UM . | Identity . | HCDR3 AA sequence . | Length . |
|---|---|---|---|---|---|---|---|---|
| Novel 1 | NJ-15 | IGHV4-59*08 | 3-22*01 | 6*03 | UM | 100,00% | ARGNYYDSSGYYYVGYYYYYMDV | 23 |
| NJ-31 | IGHV4-59*01 | 3-22*01 | 6*03 | UM | 99,65% | ARGDYYDSSGYYYVGYYYYYMDV | 23 | |
| Novel 2 | NJ-186 | IGHV3-23*01 | 3-22*01 | 4*02 | M | 96.60% | AKGYRDNYDGDQSSVFDS | 18 |
| NJ-23 | IGHV3-23*01 | 2-21*01 | 4*02 | M | 96,53% | AKGYRDNYDGDQSSVFDS | 18 | |
| Novel 3 | NJ-36 | IGHV4-34*01 | 6-6*01 | 5*02 | M | 93,33% | AKLMAGRPNWFDP | 13 |
| NJ-123 | IGHV4-34*01 | 6-6*01 | 5*02 | M | 91,67% | AKLMAGRPNWFDP | 13 |
| . | NO. . | IGHV . | IGHD . | IGHJ . | M/UM . | Identity . | HCDR3 AA sequence . | Length . |
|---|---|---|---|---|---|---|---|---|
| Novel 1 | NJ-15 | IGHV4-59*08 | 3-22*01 | 6*03 | UM | 100,00% | ARGNYYDSSGYYYVGYYYYYMDV | 23 |
| NJ-31 | IGHV4-59*01 | 3-22*01 | 6*03 | UM | 99,65% | ARGDYYDSSGYYYVGYYYYYMDV | 23 | |
| Novel 2 | NJ-186 | IGHV3-23*01 | 3-22*01 | 4*02 | M | 96.60% | AKGYRDNYDGDQSSVFDS | 18 |
| NJ-23 | IGHV3-23*01 | 2-21*01 | 4*02 | M | 96,53% | AKGYRDNYDGDQSSVFDS | 18 | |
| Novel 3 | NJ-36 | IGHV4-34*01 | 6-6*01 | 5*02 | M | 93,33% | AKLMAGRPNWFDP | 13 |
| NJ-123 | IGHV4-34*01 | 6-6*01 | 5*02 | M | 91,67% | AKLMAGRPNWFDP | 13 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal