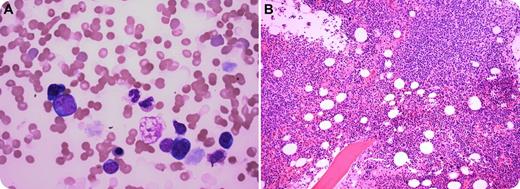
A 43-year-old man presented with fever, fatigue, and shortness of breath. Physical examination revealed bilateral axillary lymphadenopathy. Complete blood count showed hemoglobin of 9.8 g/dL, a white cell count of 4.4 × 109/L, and a platelet count of 195 × 109/L. Blood smear showed increased red blood cell agglutination, polychromasia with nucleated red cells, and atypical lymphocytosis (panel A). Hemolysis was evident, with raised serum bilirubin (2.3 mg/dL), low serum haptoglobin (4 mg/dL), high serum lactate dehydrogenase, direct Coombs test positive, and cold agglutinins (1:256). Serology studies for hepatitis B or hepatitis C were negative. Laboratory work-up detected hypergammaglobulinemia (3.9 g/dL) with increased serum immunoglobulin G (IgG) (2408 mg/dL), IgM (599 mg/dL), and IgE (175 mg/dL) with an IgG κ monoclonal paraprotein. A bone marrow biopsy revealed dense nodular atypical lymphoid infiltrates, plasmacytosis, and megakaryocytic hyperplasia (panel B). Biopsy of the axillary lymph nodes showed diffuse large B-cell lymphoma. Subsequently, the patient was discovered to be positive for HIV type 1, with a viral load of 485 315 copies per microliter, and a CD4 cell count of 215 per microliter.
All patients with unexplained cold agglutination and hypergammaglobulinemia associated with lymphoma should undergo screening for HIV infection; peripheral blood analysis may be useful in the diagnosis of marrow involvement by lymphoma.
A 43-year-old man presented with fever, fatigue, and shortness of breath. Physical examination revealed bilateral axillary lymphadenopathy. Complete blood count showed hemoglobin of 9.8 g/dL, a white cell count of 4.4 × 109/L, and a platelet count of 195 × 109/L. Blood smear showed increased red blood cell agglutination, polychromasia with nucleated red cells, and atypical lymphocytosis (panel A). Hemolysis was evident, with raised serum bilirubin (2.3 mg/dL), low serum haptoglobin (4 mg/dL), high serum lactate dehydrogenase, direct Coombs test positive, and cold agglutinins (1:256). Serology studies for hepatitis B or hepatitis C were negative. Laboratory work-up detected hypergammaglobulinemia (3.9 g/dL) with increased serum immunoglobulin G (IgG) (2408 mg/dL), IgM (599 mg/dL), and IgE (175 mg/dL) with an IgG κ monoclonal paraprotein. A bone marrow biopsy revealed dense nodular atypical lymphoid infiltrates, plasmacytosis, and megakaryocytic hyperplasia (panel B). Biopsy of the axillary lymph nodes showed diffuse large B-cell lymphoma. Subsequently, the patient was discovered to be positive for HIV type 1, with a viral load of 485 315 copies per microliter, and a CD4 cell count of 215 per microliter.
All patients with unexplained cold agglutination and hypergammaglobulinemia associated with lymphoma should undergo screening for HIV infection; peripheral blood analysis may be useful in the diagnosis of marrow involvement by lymphoma.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal