Key Points
CLEC-2 is necessary for lymphatic cell proliferation and lymph node anlage persistence after birth.
Lack of CLEC-2 expression on megakaryocytes and platelets compromises lymph node integrity in adult life.
Abstract
The importance of CLEC-2, a natural ligand/receptor for Gp38/Podoplanin, in the formation of the lymphatic vasculature has recently been demonstrated. As the development and maintenance of lymph nodes (LNs) is dependent on the formation of the lymphatic vasculature and the differentiation of Gp38/Podoplanin+ stromal cells, we investigated the role of CLEC-2 in lymphoneogenesis and LN homeostasis. Using constitutive Clec1b−/− mice, we showed that while CLEC-2 was not necessary for initiation of the LN anlage, it was required at late stages of development. Constitutive deletion of CLEC-2 induced a profound defect in lymphatic endothelial cell proliferation, resulting in lack of LNs at birth. In contrast, conditional deletion of CLEC-2 in the megakaryocyte/platelet lineage in Clec1bfl/flPF4-Cre mice led to the development of blood-filled LNs and fibrosis, in absence of a proliferative defect of the lymphatic endothelial compartment. This phenotype was also observed in chimeric mice reconstituted with Clec1bfl/flPF4-Cre bone marrow, indicating that CLEC-2 expression in platelets was required for LN integrity. We demonstrated that LNs of Clec1bfl/flPF4-Cre mice are able to sustain primary immune responses but show a defect in immune cell recirculation after repeated immunizations, thus suggesting CLEC-2 as target in chronic immune response.
Introduction
Lymph nodes (LNs) are organized anatomical structures distributed at strategic sites alongside the lymphatic vasculature that provide the hub of the acquired immune system. Their organization is supported by stromal cell populations,1,2 allowing maximal interaction between antigen-loaded dendritic cells (DCs) migrating through the afferent lymphatic vasculature and recirculating lymphocytes entering through the blood vasculature. The combination of the markers CD31 (PECAM-1), Gp38/Podoplanin, CD35, and RANKL has allowed the identification of at least 5 stromal cell populations: blood endothelial cells (BECs; Gp38−CD31+CD35−RANKL−), lymphatic endothelial cells (LECs; Gp38+CD31+CD35−RANKL−), fibroblastic reticular cells (FRCs; Gp38+CD31−CD35−RANKL−), follicular DCs (FDCs; Gp38+/−CD31−CD35+RANKL−) and marginal reticular cells (MRCs; Gp38+CD31−CD35+RANKL+).3,4 These populations are responsible for immune cell interaction and antigen presentation, ultimately providing the anatomical base for the organization of the acquired immune response.
LN development begins during embryogenesis, following precise timing according to anatomical location: the mesenteric LNs develop first, followed by the others along the anterior-posterior axis. A key event is the recruitment and clustering of the hematopoietic lymphoid tissue inducer (LTi) cells expressing lymphotoxin α1β2. Engagement by LTi cells of the lymphotoxin β receptor (LTβR) on immature stromal cells will direct their maturation to lymphoid tissue organizer (LTo) cells that regulate further LTi cell clustering and development of the anlage.5-7 The lymphatic vasculature is integral to LN structure; however, its importance in the development of the anlage remains unclear. Despite the development of the LN anlagen is synchronized with the formation of the lymph sacs, which characterize the beginning of the establishment of the lymphatic vasculature,8,9 LN formation is initiated normally in Prox-1−/− embryos which are devoid of lymph sacs and lymphatic vessels.9 Due to the early lethality of Prox-1−/− embryos, the definitive outcome of the LN anlagen, which is disorganized in the absence of the lymphatic vasculature, remains unknown. In adult LNs, the lymphatic vasculature is embedded in the LN structure and interruption of the afferent lymphatic vessels has been shown to cause LN regression and loss of high endothelial venules (HEVs).10
CLEC-2 (encoded by Clec1b), a C-type lectin-like receptor is an endogenous ligand for Gp38/Podoplanin expressed at high levels on megakaryocyte-derived platelets, inflammatory DCs, and possibly other hematopoietic cells. CLEC-2 contains a half immunoreceptor tyrosine-based activation motif (ITAM), also known as a hemITAM, and signals via the tyrosine kinase Syk,11 mediating platelet activation and thrombus formation.12-14 Deficiency in CLEC-2 or its ligand Gp38/Podoplanin results in systemic edema and abnormal lymphatic vasculature development characterized by blood-filled lymphatic vessels.15-19 These defects are also seen in mice with deletions in genes encoding CLEC-2–signaling cascade proteins (Syk, SLP-76 and PLCγ217 ), thus highlighting a role for CLEC-2 signaling in the development of the lymphatic vasculature. The molecular basis and anatomical location of the blood-lymphatic mixing has been proposed to occur at the level of the thoracic duct20 and is no longer thought to be due to a defect in separation of the lymphatic endothelial cells from the cardinal vein.21,22 Additionally, studies using a soluble form of Podoplanin (Podoplanin-Fc) suggest that inhibition of Podoplanin function inhibits lymphangiogenesis.23 Gp38/Podoplanin is expressed on different LN stromal cell populations in embryonic and adult life but the role of CLEC-2 in LN development and homeostasis has only recently been appreciated. Clec1b-deficient DCs have been shown to fail to access the Gp38+ afferent lymphatics, reducing T-cell priming and antigen response in LNs,24 while a role for CLEC-2 in HEV maintenance was reported during the revision of this manuscript.25 In our study, we took advantage of the Clec1b−/− mouse and the Clec1bfl/flPF4-Cre conditional mouse, in which Clec1b expression is selectively deleted on the megakaryocyte/platelet lineage, to dissect the role of CLEC-2 in the development of the LN anlage in the embryo and the maintenance of the LN structure and function in adult life.
Material and methods
Mice
Clec1b-deficient mice (Clec1b−/− and Clec1bfl/flPF4-Cre) have been previously described.16 Mice were bred and maintained in the Biomedical Service Unit at the University of Birmingham according to Home Office and local ethics committee regulations. Day of vaginal plug was designated as embryonic day 0 (E0). Bone marrow chimeras were generated after irradiation of C57BL/6 mice and reconstitution either with fetal liver isolated at E15.5 from Clec1b−/− or bone marrow from Clec1bfl/flPF4-Cre. Six weeks after reconstitution, animals were sacrificed and LNs removed and analyzed.
Cell isolation
Embryonic, newborn, and adult LNs, mesenteries, intestine, and lungs were isolated and disaggregated to single-cell suspensions as previously described.16 Cells were washed and resuspended in magnetic-activated cell sorting buffer for staining.
For analysis of draining and nondraining brachial LNs, individual LNs were teased apart using forceps, digested for 20 minutes at 37°C in RPMI with 0.3 mg/mL collagenase dispase and 100 μg/mL DNase I. Enzymatic digestion was stopped by addition of RPMI with 2.5 mM EDTA. Tissue suspensions were crushed through nylon mesh and a single-cell suspension collected.
LN immunization
Naive CD45.1+ SM1 cells (105) derived from spleen and a pool of peripheral LNs from Rag−/− × SM1 CD45.1+ mice were transferred IV into 6-week-old Clec1bfl/flPF4-Cre and Clec1bfl/fl control mice. The following day, mice were immunized in the front paw pad with ∼20 μg of FliC peptide precipitated with alum. For the phycoerythrin (PE) immunization, mice were immunized in the front paw pad with 10 μg of PE precipitated with alum. Seven days after immunization, draining and nondraining brachial LNs were isolated and either snap-frozen for immunofluorescence or prepared for flow cytometric analysis. For the 3-hydroxy-4-acetyl nitrophenol (NP)-CGG reimmunization experiment, mice were immunized 3 times with 10 μg of NP-CGG precipitated with alum. LN single-cell suspensions were analyzed 8 days after the last immunization.
Antibodies and flow cytometry
Single-cell suspensions were stained with directly conjugated antibodies. Anti-B220–fluorescein isothiocyanate (FITC) or -e450 (RA3-B2), anti-CD11c-PEcy7 (N418), anti-CD45-PerCPcy5.5 (30-F11), anti-IgD–Alexa 647 (11-26), anti–immunoglobulin M (IgM)–PEcy7 (11/41), CD31-FITC (390), CD45 or –allophycocyanin (APC) (30-F11), Gp38-PE (eBio8.1.1), ICAM-1–PE (YN1/1.7.4), Ter119–FITC or –PerCPCy5.5 (TER119), VCAM-1–APC (429) (eBioscience), and Ki67–Alexa 647 (B56; BD Pharmingen). Four-color flow cytometric analysis was performed using a FACSCalibur or Cyan (BD Biosciences) with forward/side scatter gates set to exclude nonviable cells. Data were analyzed with FlowJo software (TreeStar).
Immunofluorescence staining
Six-micron sections of tissue were cut by cryosectioning and stained with directly conjugated or unconjugated antibodies. Unconjugated antibodies were detected using appropriate secondary antibodies. Abs used were Gp38/podoplanin 8.1.1, CD41-FITC clone ebioMWReg30 (eBioscience), Lyve-1 (rabbit polyclonal; Abcam) or Lyve-1 eFluor 660 clone ALY7 (eBioscience), CD31-biotin or CD31-FITC clone 390 (eBioscience), CD4 Alexa Fluor 647 clone RM4-5 (BD Pharmingen), CD45R (B220) eFluor 450 clone RA3-6B2 (eBioscience), CD3e-biotin clone ebio500A2 (eBioscience), CD11c-biotin clone N418 (eBioscience), receptor activator for NF-κB ligand (RANKL)–biotin clone IK22/5 (eBioscience), CXCL13 and CCL21 (goat polyclonal; R&D Systems), FDC-M2 biotinylated (ImmunoKontact), ER-TR7 supernatant (Biogenesis), ROR γ(t) clone AFKJS-9 (eBioscience). CD31–FITC-conjugated Ab was detected using rabbit anti-FITC (Sigma-Aldrich), then goat anti-rabbit IgG-FITC (Jackson ImmunoResearch Laboratories). Lyve-1 Ab was detected using goat anti-rabbit IgG-FITC (Jackson ImmunoResearch Laboratories). CXCL13 and CCL21 Ab were detected using donkey anti-goat FITC (Jackson ImmunoResearch Laboratories) then rabbit anti-FITC (Sigma-Aldrich), followed by goat anti-rabbit IgG-FITC (Jackson ImmunoResearch Laboratories). ER-TR7 was detected using donkey anti-rat FITC or Cy3 (Jackson ImmunoResearch Laboratories). Gp38/podoplanin was detected using goat anti-hamster biotin (Cambridge Bioscience). Biotinylated antibodies were detected using streptavidin–Alexa Fluor 555 or 488 (Molecular Probes). Sections were mounted using Vectashield mounting medium (Vector Laboratories).
Image acquisition and analysis of confocal images
Confocal images were acquired using a Zeiss LSM 510 laser-scanning confocal head with a Zeiss Axio Imager Z1 microscope. Digital images were recorded and stored as digital arrays of 2048 × 2048 pixels with 8-bit sensitivity; detectors were routinely set so that intensities in each channel spanned the 0 to 255 scale optimally.
Statistical analysis
Statistical significance was determined for all analysis in Figures 1 through 5 with a 2-tailed Student t test. In Figure 6, statistical significance was determined by the 2-tailed Mann-Whitney test.
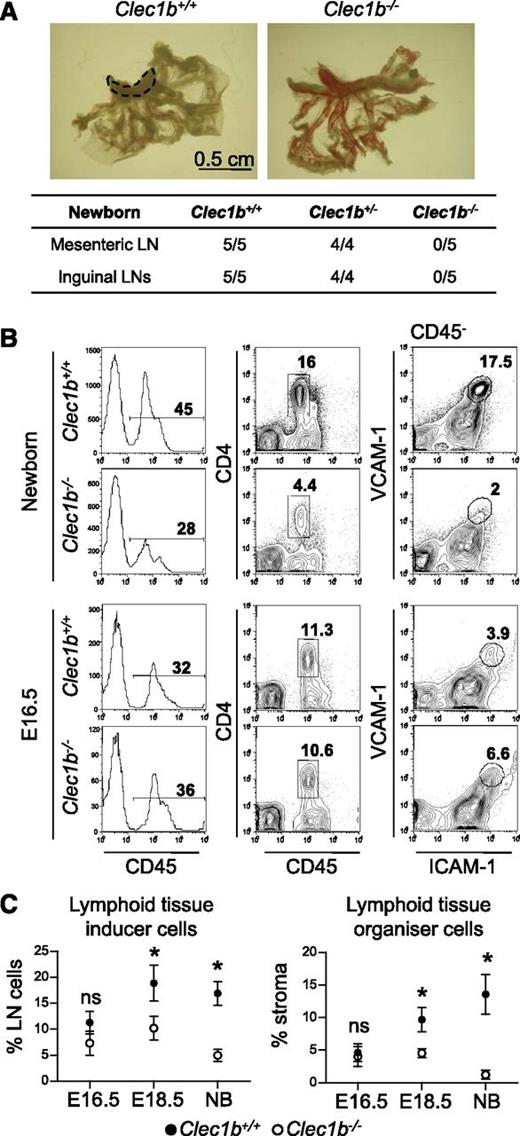
Impaired LN development in Clec1b−/− embryos. (A) Macroscopic observation of newborns Clec1b−/−, Clec1b+/−, and Clec1b+/+ littermates revealed the absence of inguinal and mesenteric LNs in Clec1b−/−. Fraction of the number of newborn mice with detectable LNs/number of mice sacrificed. (B) Flow cytometric analysis of mesenteric LN single-cell suspensions from Clec1b−/− and Clec1b+/+ littermates newborn and E16.5 stained with CD45, CD4, ICAM-1, and VCAM-1. Percentage of CD45+ hematopoietic cells is shown in the histogram (first column); percentages of CD45+CD4+ LTi cells (second column), and of ICAM-1highVAM-1high LTo cells, in the CD45− stromal fraction (third column) are shown in the dot plots. (C) Quantification of the recruitment of LTi cells (gated as shown in B second column) and of LTo cells in the CD45+ stromal fraction (gated as shown in B third column) in the LN anlage at E16.5, E18.5, and newborn stages. Data are representative of 3 to 5 embryos for each time point and phenotype across at least 2 independent experiments. Unpaired Student t test, *P < .05.
Impaired LN development in Clec1b−/− embryos. (A) Macroscopic observation of newborns Clec1b−/−, Clec1b+/−, and Clec1b+/+ littermates revealed the absence of inguinal and mesenteric LNs in Clec1b−/−. Fraction of the number of newborn mice with detectable LNs/number of mice sacrificed. (B) Flow cytometric analysis of mesenteric LN single-cell suspensions from Clec1b−/− and Clec1b+/+ littermates newborn and E16.5 stained with CD45, CD4, ICAM-1, and VCAM-1. Percentage of CD45+ hematopoietic cells is shown in the histogram (first column); percentages of CD45+CD4+ LTi cells (second column), and of ICAM-1highVAM-1high LTo cells, in the CD45− stromal fraction (third column) are shown in the dot plots. (C) Quantification of the recruitment of LTi cells (gated as shown in B second column) and of LTo cells in the CD45+ stromal fraction (gated as shown in B third column) in the LN anlage at E16.5, E18.5, and newborn stages. Data are representative of 3 to 5 embryos for each time point and phenotype across at least 2 independent experiments. Unpaired Student t test, *P < .05.
Results
Impaired LN development in Clec1b−/− embryos
To assess the effect of CLEC-2 loss on LN formation, we studied the formation of inguinal and mesenteric LNs in Clec1b−/− stillborn pups. Macroscopic analysis revealed absence of mesenteric and inguinal LNs in Clec1b−/− newborns but not in Clec1b+/− and Clec1b+/+ littermates (Figure 1A). The developmental stage of the LN anlage was assessed by flow cytometry in digested embryonic or newborn cells for the recruitment of CD45+CD4+ LTi cells and expression of ICAM-1 and VCAM-1 on CD45− stromal cells.26,27 Analysis of the mesenteric LN in newborn Clec1b−/− mice showed a fourfold reduction in the frequency of LTi cells with respect to their wild-type (WT) littermates (Figure 1B, first and second row). Concomitantly, the ICAM-1highVCAM-1high mature LTo cell compartment was dramatically reduced in Clec1b−/− mesenteric LN anlage (Figure 1B, third row). These results indicated that LN development is markedly impaired in Clec1b−/− mice (Figure 1B).
The lack of LNs observed in Clec1b−/− newborn mice could result from either an early defect or a later impairment in LN anlage development. Flow cytometric analysis of E16.5 mesenteric LN anlage showed no significant differences in the percentage of LTi cells and LTo cells between Clec1b−/− embryos and their WT littermates (Figure 1B, third and fourth row) indicating that a deficiency in CLEC-2 does not affect the initial development of mesenteric LNs. However, by E18.5 a reduction in the frequency of LTi and LTo cells in the LNs of Clec1b−/− embryos in respect to their WT littermates was observed that was even more pronounced in newborns (Figure 1C and data not shown). This indicates that CLEC-2 is required for mesenteric LN development in late embryogenesis.
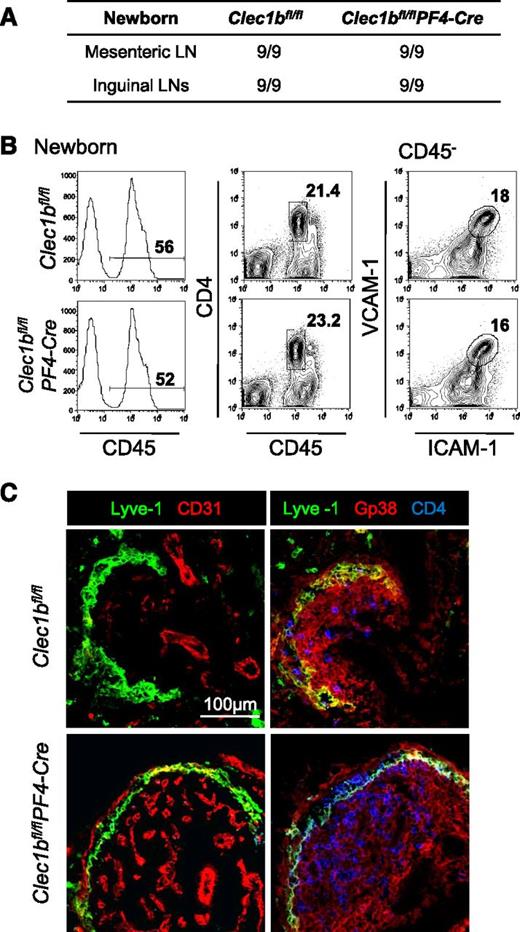
Lack of CLEC-2 expression in the megakaryocytes lineage does not affect LN development
To understand the lineage-specific requirements for CLEC-2 during LN development, we crossed mice carrying a conditional loxP-flanked allele of Clec1b (Clec1bfl/fl) with a PF4-Cre transgenic mouse line to generate Clec1bfl/flPF4-Cre mice that lack CLEC-2 expression in megakaryocytes and platelets.16 These mice retain a phenotype characterized by red blood cells filling the lymphatic vessels but were viable. Macroscopic observation revealed that, in contrast to the Clec1b−/− mice, LNs were present in the Clec1bfl/flPF4-Cre mice (Figure 2A), yet presenting a bloodied appearance.14 Flow cytometric analysis showed normal recruitment of LTi cells and maturation of the stroma into LTo cells (Figure 2B). The architecture of the LNs from Clec1bfl/flPF4-Cre newborns and Clec1bfl/fl littermates was similar, as shown by the numerous CD31+ blood vessels and normal development of the Gp38+Lyve-1+ subcapsular sinus (Figure 2C). These differences suggest that, while CLEC-2 expression is necessary for LN embryological development, its source at this stage may derive from cells not belonging to the megakaryocyte lineage. We ruled out that the less severe phenotype observed in the Clec1bfl/flPF4-Cre embryos was the consequence of a delay in the deletion of CLEC-2 on platelets due to the time needed for PF4 induction of the Cre enzyme in the embryo. Indeed, we showed that CLEC-2 is absent on platelets from E11.5 onwards in Clec1bfl/flPF4-Cre mice confirming the efficacy of CLEC-2 deletion at this stage (supplemental Figure 1, available on the Blood Web site).
Normal LN development in Clec1bfl/flPF4-Cre newborns. (A) Macroscopic observation of newborns Clec1bfl/flPF4-Cre and Clec1bfl/fl littermates revealed the presence of inguinal and mesenteric LNs in Clec1bfl/flPF4-Cre newborns. Fraction of number of newborn mice with detectable LN/number of mice sacrificed. (B) Flow cytometric analysis of mesenteric LN single-cell suspensions from Clec1bfl/flPF4-Cre and Clec1bfl/fl newborn littermates stained with CD45, CD4, ICAM-1, and VCAM-1. Percentage of CD45+ hematopoietic cells is shown in the histogram; percentages of CD45+CD4+ LTi cells (second column) and of ICAM-1highVAM-1high LTo cells in the CD45− stromal fraction (third column) are shown in the dot plots. (C) Immunofluorescence staining of sections from newborn mesenteric LNs showing the CD31+ blood endothelial vasculature in red and the Lyve-1+ LECs in green forming the subcapsular sinus (first column) and the Gp38+ stromal cell compartment in red and CD4+ cells in blue (second column) in Clec1bfl/fl (upper row) and Clec1bfl/flPF4-Cre littermates (lower row).
Normal LN development in Clec1bfl/flPF4-Cre newborns. (A) Macroscopic observation of newborns Clec1bfl/flPF4-Cre and Clec1bfl/fl littermates revealed the presence of inguinal and mesenteric LNs in Clec1bfl/flPF4-Cre newborns. Fraction of number of newborn mice with detectable LN/number of mice sacrificed. (B) Flow cytometric analysis of mesenteric LN single-cell suspensions from Clec1bfl/flPF4-Cre and Clec1bfl/fl newborn littermates stained with CD45, CD4, ICAM-1, and VCAM-1. Percentage of CD45+ hematopoietic cells is shown in the histogram; percentages of CD45+CD4+ LTi cells (second column) and of ICAM-1highVAM-1high LTo cells in the CD45− stromal fraction (third column) are shown in the dot plots. (C) Immunofluorescence staining of sections from newborn mesenteric LNs showing the CD31+ blood endothelial vasculature in red and the Lyve-1+ LECs in green forming the subcapsular sinus (first column) and the Gp38+ stromal cell compartment in red and CD4+ cells in blue (second column) in Clec1bfl/fl (upper row) and Clec1bfl/flPF4-Cre littermates (lower row).
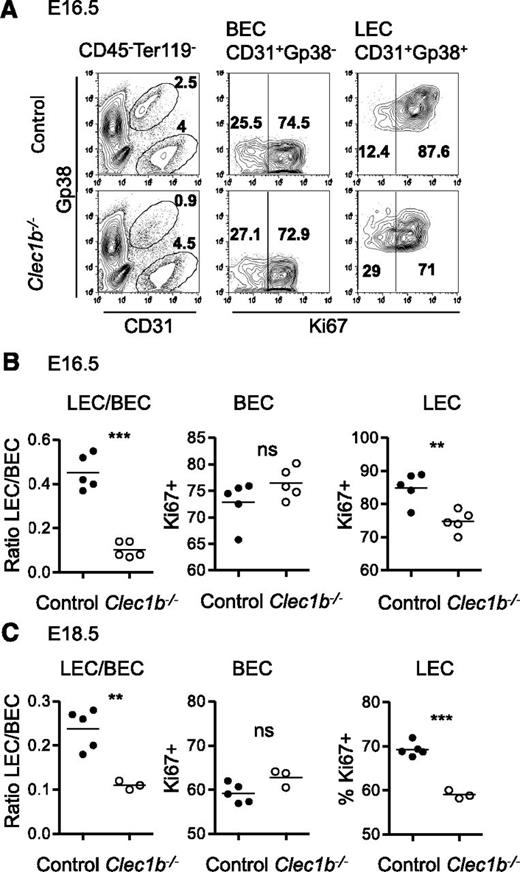
Lymphatic endothelial cells from Clec1b−/− embryos have a proliferative defect
We recently demonstrated that Clec1b−/− embryos have a defect in the number of LECs and a decrease in the LEC:BEC ratio in the intestine, mesenteries, and lungs, as well as blood-lymphatic mixing.16 To better understand the function of CLEC-2 in endothelial cells, we analyzed the proliferation status of the LEC and BEC populations in Clec1b−/−and WT littermate embryos and newborns, focusing on the intestine, from which we could recover the higher number of LEC in embryonic life. The LEC compartment in the intestine is significantly reduced in E16.5 Clec1b−/− embryos (Figure 3A), as shown by a decreased LEC:BEC ratio in E16.5 to 18.5 Clec1b−/− embryos compared with control littermates (Figure 3B-C). The LEC compartment, but not the BEC compartment, showed a decrease in the frequency of proliferating cells in E16.5 Clec1b−/− mice compared with littermates as shown by Ki67 staining (Figure 3A). Further analysis of the percentage of proliferating LECs at E16.5 and E18.5 showed a statistically significant decrease in Clec1b−/− embryos compared with controls (Figure 3B-C). Taken together, these results indicated a specific role for CLEC-2 in the normal proliferation of LECs but not of BECs.
Impaired LEC proliferation in Clec1b−/− embryos. (A) Flow cytometric analysis of intestine single-cell suspensions from Clec1b−/− and control littermates at E16.5 stained with CD45, Ter119, Gp38, CD31, and Ki67. The percentages of CD31+Gp38− BEC and of CD31+Gp38+ LEC in the CD45−Ter119− stromal fraction are indicated in the dot plots of the first column. The percentages of Ki67+ in the BEC and LEC compartment are shown in the dot plots of the second and third columns. (B-C) Quantifications of the ratio of LEC:BEC and of the ratio of Ki67+ in the BEC and LEC compartments are shown in the first, second, and third charts at E16.5 (B) and E18.5 (C) in the intestine. Unpaired Student t test, **P < .01, ***P < .005.
Impaired LEC proliferation in Clec1b−/− embryos. (A) Flow cytometric analysis of intestine single-cell suspensions from Clec1b−/− and control littermates at E16.5 stained with CD45, Ter119, Gp38, CD31, and Ki67. The percentages of CD31+Gp38− BEC and of CD31+Gp38+ LEC in the CD45−Ter119− stromal fraction are indicated in the dot plots of the first column. The percentages of Ki67+ in the BEC and LEC compartment are shown in the dot plots of the second and third columns. (B-C) Quantifications of the ratio of LEC:BEC and of the ratio of Ki67+ in the BEC and LEC compartments are shown in the first, second, and third charts at E16.5 (B) and E18.5 (C) in the intestine. Unpaired Student t test, **P < .01, ***P < .005.
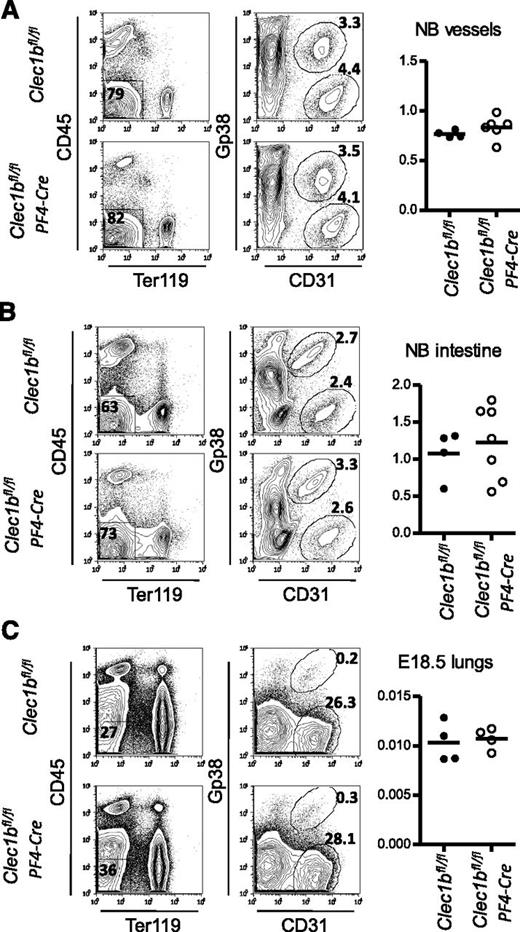
CLEC-2 expression in megakaryocytes/platelets is not required to maintain a normal LEC:BEC ratio during embryogenesis
To dissect the differences observed in the development of the LN anlage between the Clec1b−/− and Clec1bfl/flPF4-Cre mouse models, we assessed the LEC:BEC ratio in the Clec1bfl/flPF4-Cre embryos and newborn mice. Tissue isolated from the mesenteries (LNs being removed), intestine, and lungs was digested and cell suspensions were stained for CD45, Ter119, Gp38, and CD31. We could not detect significant differences in the LEC:BEC ratio of the mesenteries, intestine, or lungs between Clec1bfl/flPF4-Cre and their littermate controls, suggesting that CLEC-2 expressed by platelets/megakaryocytes was not necessary for the maintenance of a normal LEC:BEC ratio at these sites (Figure 4).
Normal LEC:BEC ratio in Clec1bfl/flPF4-Cre embryos and newborns. (A-C) Flow cytometric analysis of newborn mesenteric vessels (without the LNs, A), newborn intestine (B), and E18.5 lungs (C), single-cell suspensions from Clec1bfl/flPF4-Cre and Clec1bfl/fl control littermates, stained with CD45, Ter119, Gp38, and CD31. Percentages of CD31+Gp38− BEC and of CD31+Gp38+ LEC in the CD45−Ter119− stromal fraction are indicated in the dot plots of the second columns. Quantification of the ratios of LEC:BEC are shown on the charts.
Normal LEC:BEC ratio in Clec1bfl/flPF4-Cre embryos and newborns. (A-C) Flow cytometric analysis of newborn mesenteric vessels (without the LNs, A), newborn intestine (B), and E18.5 lungs (C), single-cell suspensions from Clec1bfl/flPF4-Cre and Clec1bfl/fl control littermates, stained with CD45, Ter119, Gp38, and CD31. Percentages of CD31+Gp38− BEC and of CD31+Gp38+ LEC in the CD45−Ter119− stromal fraction are indicated in the dot plots of the second columns. Quantification of the ratios of LEC:BEC are shown on the charts.
Lack of CLEC-2 expression by megakaryocytes/platelets led to blood-filled LNs in Clec1bfl/flPF4-Cre adult mice
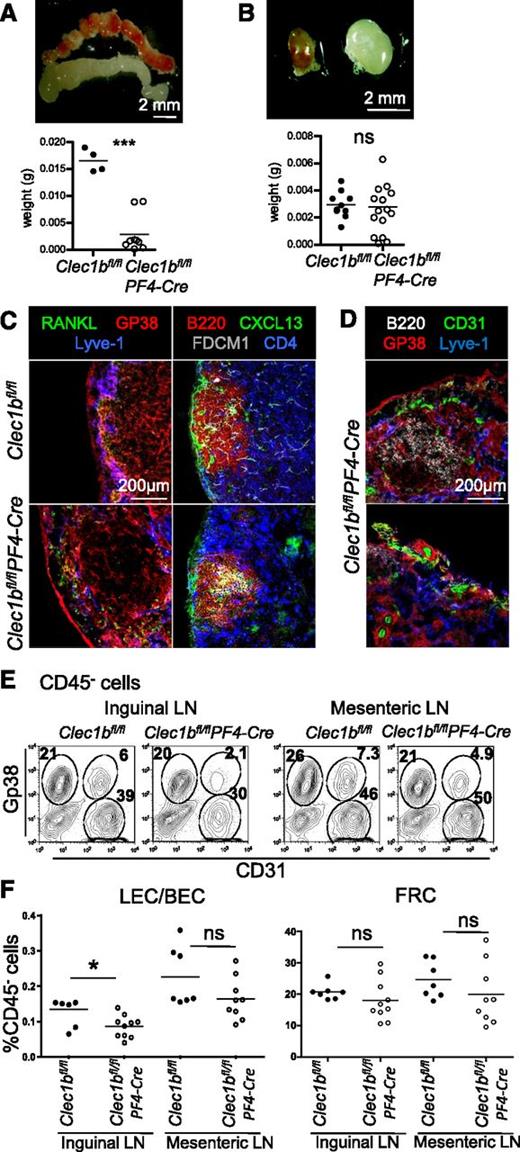
The generation of the Clec1bfl/flPF4-Cre mouse model allowed us to dissect the role of megakaryocyte/platelets derived CLEC-2 in the maintenance of adult LN structure and function, which was not possible in Clec1b−/− mice. All LNs and Peyer patches examined from the Clec1bfl/flPF4-Cre mouse strain were filled with red blood cells (Figure 5A-B and data not shown) demonstrating that the absence of CLEC-2 expression by megakaryocytes/platelets is instrumental in maintaining vascular integrity in these structures.16 Furthermore, this phenotype was associated with a significant defect in size and weight of mesenteric LNs (Figure 5A), whereas inguinal LNs showed a large degree of variability in these parameters (Figure 5B). Histological examination of the largest LNs in the Clec1bfl/flPF4-Cre mice showed a generally preserved microscopic structure with normal B-/T-cell segregation and preserved marginal sinus (Figure 5C). In contrast, the smallest LNs (both mesenteric and inguinal) appeared fibrotic and showed a degree of histological disorganization and subversion of the follicular structure (Figure 5D).
Impaired maintenance of the LNs in adults Clec1b−/−PF4-Cre. (A-B) Macroscopic appearance and weight of mesenteric (A) and inguinal (B) LNs from adult Clec1bfl/flPF4-Cre and Clec1bfl/fl control littermates. (C) Immunofluorescence staining of a section of adult LN from Clec1bfl/flPF4-Cre and Clec1bfl/fl control littermates stained for RANKL in green, Gp38/Podoplanin in red, and Lyve-1 in blue (first column) and B220 in red, CXCL13 in green, FDCM1 in gray, and CD4 in blue (second column), showing preserved LN structure in large inguinal Clec1bfl/flPF4-Cre LNs. (D) Immunofluorescence staining of section of fibrotic LNs from Clec1bfl/flPF4-Cre adult mice stained for B220 in white, CD31 in green, Gp38/Podoplanin in red, and Lyve-1 in blue. (E) Flow cytometric analysis of adult inguinal (first column) and mesenteric (second column) LN single-cell suspensions from Clec1bfl/fl control and Clec1bfl/flPF4-Cre littermates, stained with CD45, Gp38, and CD31. Percentages of CD31+Gp38− BEC, CD31+Gp38+ LEC, and CD31−Gp38+ FRC in the CD45− stromal fraction are indicated in the dot plots. (F) Quantification of the ratios of LEC:BEC (top chart) and percentages of FRC in the CD45− cell fraction (bottom chart) are shown. Unpaired Student t test, *P < .05, ***P < .001.
Impaired maintenance of the LNs in adults Clec1b−/−PF4-Cre. (A-B) Macroscopic appearance and weight of mesenteric (A) and inguinal (B) LNs from adult Clec1bfl/flPF4-Cre and Clec1bfl/fl control littermates. (C) Immunofluorescence staining of a section of adult LN from Clec1bfl/flPF4-Cre and Clec1bfl/fl control littermates stained for RANKL in green, Gp38/Podoplanin in red, and Lyve-1 in blue (first column) and B220 in red, CXCL13 in green, FDCM1 in gray, and CD4 in blue (second column), showing preserved LN structure in large inguinal Clec1bfl/flPF4-Cre LNs. (D) Immunofluorescence staining of section of fibrotic LNs from Clec1bfl/flPF4-Cre adult mice stained for B220 in white, CD31 in green, Gp38/Podoplanin in red, and Lyve-1 in blue. (E) Flow cytometric analysis of adult inguinal (first column) and mesenteric (second column) LN single-cell suspensions from Clec1bfl/fl control and Clec1bfl/flPF4-Cre littermates, stained with CD45, Gp38, and CD31. Percentages of CD31+Gp38− BEC, CD31+Gp38+ LEC, and CD31−Gp38+ FRC in the CD45− stromal fraction are indicated in the dot plots. (F) Quantification of the ratios of LEC:BEC (top chart) and percentages of FRC in the CD45− cell fraction (bottom chart) are shown. Unpaired Student t test, *P < .05, ***P < .001.
In keeping with the results obtained in the embryos, stromal cell digestion and fluorescence-activated cell sorter analysis of Clec1bfl/flPF4-Cre LN showed only a mild defect in the LEC number (Figure 4) resulting in the overall maintenance of the LEC:BEC ratio (Figure 5E-F). No significant differences in the frequency of the Gp38+ FRC and MRC cells were present between LNs from the Clec1bfl/flPF4-Cre mice and their control littermates (Figure 5E-F and data not shown). These results suggest that, while the lack of CLEC-2 expression on megakaryocyte/platelets has a strong impact on the stability of the blood and lymphatic vascular bed and LN morphology, this is not reflected in a significant impairment of the lymphatic and stromal cell components.
Of interest, spleens isolated from Clec1bfl/flPF4-Cre mice showed enlarged size as compared with the littermate controls (supplemental Figure 2A). Nonetheless, histological examination of this tissue did not show major differences in spleen architecture and organization (supplemental Figure 2B).
Loss of CLEC-2 expression in megakaryocytes/platelets does not compromise primary immune response
To investigate whether Clec1bfl/flPF4-Cre LNs maintain a normal immunological function, we analyzed the lymphoid compartment under resting conditions and postimmunization. No significant differences were observed under resting conditions between Clec1bfl/flPF4-Cre and Clec1bfl/fl littermates in the frequency of T lymphocytes, B lymphocytes, or DC distribution (supplemental Figure 3).
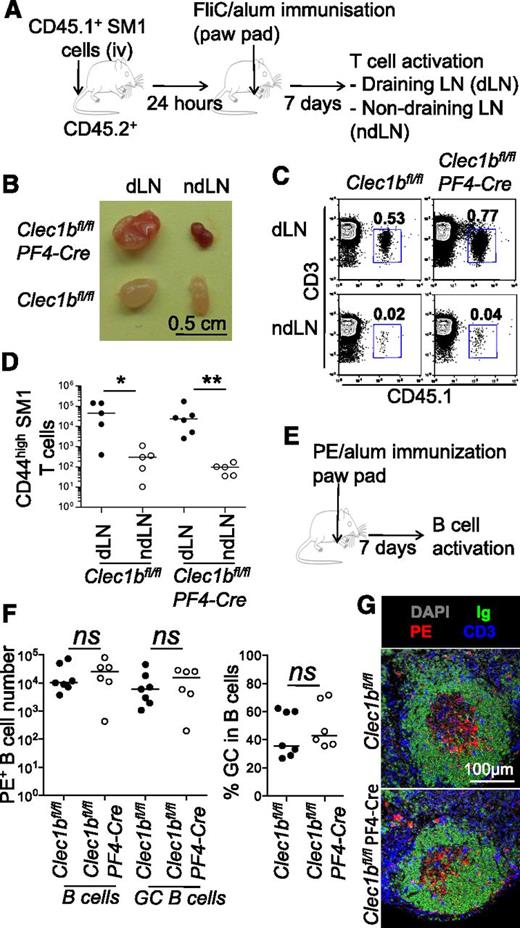
To test whether Clec1bfl/flPF4-Cre LNs were able to support normal CD4 T-cell responses, 105 CD45.1+ SM1 TCR-transgenic T cells (which recognize FliC peptide) were transferred IV into CD45.2+Clec1bfl/flPF4-Cre mice. The following day, these mice were immunized with 20 μg of alum-precipitated FliC peptide in the front paw pad, a site that drains to the brachial LN. Seven days postimmunization, numbers of CD45.1+ SM1 T cells were analyzed in draining and nondraining brachial LNs (Figure 6A). In both control Clec1bfl/fl and Clec1bfl/flPF4-Cre mice, draining LNs were enlarged (Figure 6B) and contained a significantly expanded number of CD45.1+CD3+CD44+ SM1 cells compared with nondraining LNs (Figure 6C-D), indicating the normal expansion of CD4+ T cells in these mice. To further investigate the ability of Clec1bfl/flPF4-Cre LNs to support adaptive immune response, the endogenous PE-specific B-cell response was assessed after immunization in the paw pad with 10 μg of PE precipitated with alum (Figure 6E). In both control Clec1bfl/fl and Clec1bfl/flPF4-Cre mice, the number of PE-specific B cells was comparable, indicating the expansion of these cells was not perturbed (Figure 6F). Furthermore, no defect in the development of germinal center (GC) B cells was apparent with both Clec1bfl/fl and Clec1bfl/flPF4-Cre brachial LNs containing comparable numbers and proportions of GL7+CD38− PE-specific B cells (Figure 6F). These PE-specific GCs also appeared comparable when assessed by immunofluorescence (Figure 6G). Combined, these data indicate that primary B- and T-cell responses in Clec1bfl/flPF4-Cre LNs are normal.
Normal primary immune response in Clec1b−/−PF4-Cre adult mice. (A) CD45.1+ SM1 cells (105) were transferred into CD45.2+Clec1bfl/flPF4-Cre and Clec1bfl/fl mice, which were immunized the following day with ∼20 μg of alum-precipitated FliC peptide in the front paw pad. After 7 days, numbers of CD45.1+ SM1 T cells were analyzed in draining and nondraining contralateral brachial LNs. (B) Macroscopic appearance of draining (left) and nondraining (right) LNs from Clec1bfl/flPF4-Cre (top) and Clec1bfl/fl (bottom) littermates. (C) Flow cytometric analysis on the single-cell suspensions of the draining (first row) and nondraining (second row) brachial LNs of Clec1bfl/fl control and Clec1bfl/flPF4-Cre littermates showing CD45.1+CD3+ SM1 cells. Percentages of CD45.1+CD3+ SM1 cells are indicated in the dot plots. (D) Chart showing the number of SM1 cells in the draining and nondraining brachial LNs of Clec1bfl/flPF4-Cre and Clec1bfl/fl littermates. Two-tailed Mann-Whitney test, *P < .05, **P < .01. (E) Mice were immunized with PE cells in the front paw pad. After 7 days, numbers of PE+ B cells and GC B cells were analyzed in draining LNs. (F) Chart showing the number of PE+B220+ B cells and PE+ B220+GL7+CD38− GC B cells (left) and the percentages of GC B cells in the B-cell populations (right) in the draining brachial LNs of Clec1bfl/flPF4-Cre and Clec1bfl/fl littermates. Unpaired Student t test; ns, nonsignificant. (G) Immunofluorescence analysis of sections of the draining LNs of Clec1bfl/flPF4-Cre and Clec1bfl/fl littermates mice stained with DAPI in gray and for IgD in green, PE in red, and CD3 in blue.
Normal primary immune response in Clec1b−/−PF4-Cre adult mice. (A) CD45.1+ SM1 cells (105) were transferred into CD45.2+Clec1bfl/flPF4-Cre and Clec1bfl/fl mice, which were immunized the following day with ∼20 μg of alum-precipitated FliC peptide in the front paw pad. After 7 days, numbers of CD45.1+ SM1 T cells were analyzed in draining and nondraining contralateral brachial LNs. (B) Macroscopic appearance of draining (left) and nondraining (right) LNs from Clec1bfl/flPF4-Cre (top) and Clec1bfl/fl (bottom) littermates. (C) Flow cytometric analysis on the single-cell suspensions of the draining (first row) and nondraining (second row) brachial LNs of Clec1bfl/fl control and Clec1bfl/flPF4-Cre littermates showing CD45.1+CD3+ SM1 cells. Percentages of CD45.1+CD3+ SM1 cells are indicated in the dot plots. (D) Chart showing the number of SM1 cells in the draining and nondraining brachial LNs of Clec1bfl/flPF4-Cre and Clec1bfl/fl littermates. Two-tailed Mann-Whitney test, *P < .05, **P < .01. (E) Mice were immunized with PE cells in the front paw pad. After 7 days, numbers of PE+ B cells and GC B cells were analyzed in draining LNs. (F) Chart showing the number of PE+B220+ B cells and PE+ B220+GL7+CD38− GC B cells (left) and the percentages of GC B cells in the B-cell populations (right) in the draining brachial LNs of Clec1bfl/flPF4-Cre and Clec1bfl/fl littermates. Unpaired Student t test; ns, nonsignificant. (G) Immunofluorescence analysis of sections of the draining LNs of Clec1bfl/flPF4-Cre and Clec1bfl/fl littermates mice stained with DAPI in gray and for IgD in green, PE in red, and CD3 in blue.
Platelet CLEC-2 regulates LN function and stability in adult life
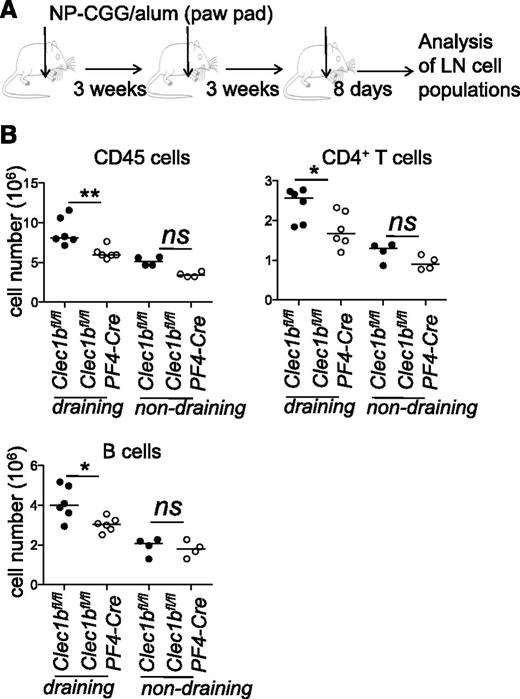
A recent study demonstrated that CLEC-2 expression on platelets is critical for the maintenance of the integrity of HEVs postimmune responses and its loss resulted in bleeding of peripheral LNs after immunization.25 To test whether the loss of HEV integrity could affect the long-term B- and T-cell recirculation in the LN, we studied lymphocyte recruitment in Clec1bfl/flPF4-Cre mice after several rounds of immunization. Mice were immunized in the front paw pad, with 10 μg of alum-precipitated NP-CGG on day 0, day 21, and day 42. Eight days after the last challenge, numbers of B and T cells were analyzed in the draining brachial LNs (Figure 7A). We demonstrated that repeated immunization gave rise to a reduced number of naive CD4+ T cells and B cells in the LNs of Clec1bfl/flPF4-Cre mice compared with control Clec1bfl/fl mice (Figure 7B). This defect was not seen in nonimmunized mice, indicating that loss of platelet CLEC-2 leads to an erosion in the LN capacity to recruit more of B and T cells upon repeated immunizations.
Defect in the recirculation of B and T cells post-reimmunization. (A) Clec1bfl/flPF4-Cre and Clec1bfl/fl mice were immunized with 10 μg of NP-CGG precipitated with alum on day 0, day 21, and day 42 in the front paw pad. (B) After 8 days, flow cytometric analysis was performed on the single-cell suspensions of the draining and nondraining brachial LNs of Clec1bfl/fl control (●) and Clec1bfl/flPF4-Cre (○) littermates, stained with CD45, CD4, CD19. Absolute numbers of CD45+ cells, CD4+ T cells, and of CD19+ B cells are indicated in the dot plots. Unpaired Student t test, *P < .05, **P < .01.
Defect in the recirculation of B and T cells post-reimmunization. (A) Clec1bfl/flPF4-Cre and Clec1bfl/fl mice were immunized with 10 μg of NP-CGG precipitated with alum on day 0, day 21, and day 42 in the front paw pad. (B) After 8 days, flow cytometric analysis was performed on the single-cell suspensions of the draining and nondraining brachial LNs of Clec1bfl/fl control (●) and Clec1bfl/flPF4-Cre (○) littermates, stained with CD45, CD4, CD19. Absolute numbers of CD45+ cells, CD4+ T cells, and of CD19+ B cells are indicated in the dot plots. Unpaired Student t test, *P < .05, **P < .01.
Finally, to evaluate whether the histological defects observed in the Clec1bfl/flPF4-Cre were constitutive or determined by the continuous requirement of megakaryocyte-derived CLEC-2 for LN maintenance, we generated bone marrow chimeras reconstituted with Clec1b−/− fetal liver cells or Clec1bfl/flPF4-Cre bone marrow. Six weeks after reconstitution, both chimeras but not controls, showed the development of a blood-filled lymphatic phenotype, reminiscent of the Clec1bfl/flPF4-Cre mice (supplemental Figure 4A and data not shown). Accordingly, histological characterization of the LNs showed variable defects in LN architecture indicating the requirement of platelet/megakaryocyte-derived CLEC-2 for the maintenance of the LN structure (supplemental Figure 4B). This defect was accompanied by a defect in recruitment of both CD4+ and CD8+ T cells in the LN postreconstitution with Clec1bfl/flPF4-Cre bone marrow, suggesting that CLEC-2 was also important for the recovery of LN homeostasis after irradiation damage (supplemental Figure 4C).
Discussion
In this study, by using both Clec1b−/− and Clec1bfl/flPF4-Cre mouse models, in which Clec1b is either constitutively deleted on all cells or selectively on megakaryocytes and platelets, we demonstrated 2 distinct and nonredundant roles for CLEC-2 in lymphangiogenesis during embryogenesis and in LN homeostasis in adult life. We showed that constitutive lack of CLEC-2 expression determines defective lymphatic cell proliferation resulting in impaired development of the lymphatic vascular structures and involution of the LN anlagen in the embryo. In contrast, the deletion of CLEC-2 on the megakaryocyte/platelet lineage as in Clec1bfl/flPF4-Cre mice allows formation of blood-filled LNs. We showed that absence of CLEC-2 on the megakaryocyte lineage in adult LN does not impair LN primary immune response, but determines long-term impairment in lymphocyte recruitment, ultimately indicating a role for CLEC-2 in the regulation of acquired immune response (see model, supplemental Figure 5).
Formation and maintenance of a functional lymphatic bed is critical for LN homeostasis in adult life.28 However, due to the early lethality of knockout mice characterized by impaired formation of the lymphatic vessels, the requirement of the lymphatic vasculature for LN anlage development is still subject to debate. The 2 knockout mouse models used in this study showed different degrees of malformation in the lymphatic vasculature with a lymphatic phenotype characterized by a reduced number of LEC forming in the Clec1b−/− embryos and a less severe phenotype with no impairment of the LEC number in Clec1bfl/flPF4-Cre embryos and newborns. Strikingly, the most severe lymphatic phenotype observed in Clec1b−/− embryo was associated with regression of inguinal and mesenteric LNs in the late embryos and newborns. This result reinforces and complements previous findings showing a normal initiation of LN anlage formation in E14.5 Prox-1−/− embryos (devoid of lymph sacs), and the presence of smaller LN anlagen in Prox1fl/fl/Tie2Cre E17.5 embryos in which conditional deletion of Prox-1 in LEC progenitors led to small and defective lymph sacs.29 Interestingly, in both Clec1b−/− and Prox1fl/fl/Tie2Cre embryos, even though LTi cells were recruited into the LN anlagen, mature LTo cells fail to persist, suggesting that a normal lymphatic vasculature is critical for the stabilization and persistence of the LN anlage stroma.
In this study, we confirmed and extended previous findings demonstrating the nonredundant role of Clec1b in the regulation of LEC proliferation.16 While our results suggest that this function is mediated in embryonic life by a cell type that does not belong to the megakaryocyte line (as Clec1bfl/flPF4-Cre adult mice do not share this defect), we have not been able so far to detect expression of CLEC-2 on cells not belonging to the megakaryocyte/platelet or DC lineage (G.E.D. and K.L., manuscript in preparation).
Upon immunization, draining LNs undergo dramatic changes of the vascular and lymphatic beds30 in which the axis Gp38/Podoplanin/CLEC-2 might be involved at different levels.31 Herzog et al demonstrated that platelets CLEC-2 is necessary to maintain HEV stability postlymphocyte migration.25 In this manuscript, the author did not report on the impact of the loss of CLEC-2 on the immune response. Here we expand these observations and explore their functional relevance demonstrating that, while loss of CLEC-2 has no direct immunological consequences in the immune responses upon single immunization, LN status after chronic antigenic stimulation is largely impaired when CLEC-2 expression on platelets is missing. We showed that, in resting conditions, the size of LNs isolated from Clec1bfl/flPF4-Cre mice are characterized by a high degree of variability. Nonetheless, no significant differences in lymphocyte composition and no defects in T- and B-cell immune responses upon primary immunization were observed in Clec1bfl/flPF4-Cre LNs. On the contrary, repeated immunization of Clec1bfl/flPF4-Cre mice led to an erosion in naive B- and T-cell LN content, thus indicating that the role of CLEC-2 in LN maintenance becomes critical in conditions of repeated antigenic challenge.
Chronic antigenic stimulation is believed to represent a key event in the formation of ectopic lymphoid organs in autoimmune conditions. At these sites, HEVs have been described that are instrumental for naive and central memory cell recirculation.32 Here, we propose that blockage of CLEC-2 activity in these conditions could represent a valid therapeutic approach, impairing lymphocyte migration and inducing ectopic lymphoid organ involution.
During the revision of this work, a manuscript describing CLEC-2 requirement to maintain lymphatic/blood system separation throughout life was published.22 Here we expand this observation demonstrating that CLEC-2 expression is required for the maintenance of the immune response in adult life, as reconstitution of WT mice with Clec1bfl/flPF4-Cre bone marrow but is associated with a significant decrease in T-cell number and disturbed histological appearance of the LNs.
While further clarifications on the role of CLEC-2/Podoplanin interaction in chronic inflammation are needed, we are confident that this work establishes the functional role of CLEC-2 in LN development, maintenance, and physiological immune response.
The online version of this article contains a data supplement.
There is an Inside Blood commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We are grateful to the personnel of the Biomedical Services Unit of the University of Birmingham for taking care of our animal colonies.
C.B. was supported by the European Union FP7 integrated project INFLACARE (J.H.C.). B.A.F. and S.P.W. are supported by the Wellcome Trust (088410).
F.B. is a Wellcome Trust Fellow. S.P.W. holds a British Heart Foundation (BHF) Chair (CH/03/003).
Authorship
Contribution: C.B. and F.B. designed the research, analyzed data, and wrote the manuscript; S.N. performed research, analyzed data, and contributed to manuscript writing; B.A.F., D.R.W., K.L., G.E.D., and C.L.M. performed experimental work and analyzed data; and S.P.W., J.H.C., and C.D.B. contributed to research design and manuscript writing.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
The current affiliation for C.B. is University of Edinburgh/BHF Centre for Cardiovascular Sciences, University of Edinburgh, Edinburgh, United Kingdom. The University of Edinburgh is a charitable body, registered in Scotland (SC005336).
Correspondence: Francesca Barone, School of Immunity and Infection, College of Medical and Dental Sciences, University of Birmingham, Birmingham, United Kingdom; e-mail: f.barone@bham.ac.uk; and Cecile Benezech, University of Edinburgh/BHF Centre for Cardiovascular Sciences, University of Edinburgh, Edinburgh, EH16 4TJ, United Kingdom; e-mail: cbenezec@staffmail.ed.ac.uk.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal