Key Points
Once-daily oral avatrombopag dose-dependently raised PCs over 28 days, with stable counts maintained over a 24-week extension.
Low rates of severe AEs and study drug discontinuations due to AEs occurred despite dose increases in maintenance.
Abstract
Stimulation of platelet production by thrombopoietin-receptor agonists (TPO-RAs) is an effective second-line treatment in immune thrombocytopenia (ITP). This 28-day phase 2 study assigned subjects with ITP of ≥3 months to once-daily oral avatrombopag (2.5, 5, 10, or 20 mg), an investigational nonpeptide TPO-RA active in humans, or placebo; subjects completing randomized treatment could enroll in a 24-week extension study. Of 64 randomized subjects, 13% (avatrombopag 2.5 mg), 53% (5 mg), 50% (10 mg), and 80% (20 mg), vs 0% for placebo, achieved a platelet count (PC) response of ≥50 × 109/L with ≥20 × 109/L increase above baseline at day 28. Fifty-three subjects (83%) entered the extension: 52% and 76% had a durable (PC response at ≥75% of their platelet assessments over the last 14 weeks) and overall (stable response or response at any ≥2 consecutive visits) response, respectively. All subjects experienced ≥1 adverse event (AE) (most commonly fatigue, headache, and epistaxis); 19% (n = 12) reported ≥1 serious AE; 10 (16%) withdrew due to an AE (5 due to increased PC). Avatrombopag was active and generally well tolerated, with PC response rates and AE incidence comparable with other TPO-RAs. These studies were registered at www.clinicaltrials.gov as #NCT00441090 and #NCT00625443.
Introduction
Immune thrombocytopenia (ITP) is characterized by autoantibody-mediated destruction of platelets and impairment of platelet production. These dual effects often result in severe thrombocytopenia and a concomitant predisposition to bleeding, with associated morbidity and mortality.1-3 Primary ITP is defined as isolated immune-mediated thrombocytopenia (peripheral blood platelet count [PC] <100 × 109/L) in the absence of other causes of thrombocytopenia.4 ITP may be asymptomatic in many affected individuals, but an increased risk of bleeding and potentially fatal hemorrhage occurs in those with a PC <30 × 109/L, especially in those aged >60 years or with other contributing factors.5
First-line therapeutic approaches for subjects with ITP include corticosteroids and/or intravenous immunoglobulins (and intravenous anti-D where available), which help to reduce the rate of immune-mediated platelet destruction. Unfortunately, most subjects experience recurrence of their thrombocytopenia once these agents are tapered or withdrawn. Subsequent treatment is guided by individualized application of clinical practice guidelines,4,6,7 and options include splenectomy, anti-CD20 agents such as rituximab, immunosuppressive agents, and thrombopoietic agents. Each of these treatments has unique benefits, limitations, tolerability considerations, and risks, with key issues including efficacy, effects on bleeding per se, morbidity, and cost.8-10
In contrast to well-established therapies that focus on mitigating platelet destruction, stimulation of thrombopoiesis is a newer approach.10 Two thrombopoietin-receptor agonists (TPO-RAs), eltrombopag and romiplostim, have been approved for the second-line treatment of chronic ITP. Both are effective in treating chronic ITP but have practical limitations; currently, in the United States, romiplostim must be given subcutaneously by a health care professional, and eltrombopag has important dietary restrictions as to when it can be taken relative to food intake.11,12 Hence, interest remains high in developing TPO-RAs for the treatment of ITP.
Avatrombopag (E5501; formerly YM477 and AKR 501) is a new, investigational, orally administered, nonpeptide TPO-RA. It is believed to mimic the biological effects of TPO in vitro and in vivo and was shown to increase PC in both animal models and healthy human volunteers.13-15 Like eltrombopag, avatrombopag is thought to bind to the transmembrane domain of the TPO receptor, which is different from the binding site of native TPO and romiplostim. Avatrombopag species specificity (only humans and chimpanzees) is attributed to the presence of histidine rather than lysine at position 499 of the TPO receptor. Avatrombopag is taken once daily and lacks significant food interactions.
Here, we report the results of sequential phase 2 studies of avatrombopag: a 28-day, double-blind, randomized study and a follow-on 24-week open-label extension study. These are the first studies to examine the efficacy and safety of once-daily avatrombopag for the treatment of ITP.
Methods
Study design
Study 003 (clinicaltrials.gov identifier #NCT00441090) involved 19 centers in the United States and was a phase 2, double-blind, randomized, dose-ranging, placebo-controlled, parallel-group trial of avatrombopag administered orally for 4 weeks. Subjects completing their assigned treatment in the randomized study were eligible to enroll in the extension study 004, a 24-week, phase 2 study across 17 centers (#NCT00625443). Both studies were conducted following approval by the independent ethics committees of participating centers and in accordance with the Declaration of Helsinki, and all subjects provided written informed consent.
Subjects
For the randomized study, eligible subjects
were aged ≥18 years;
had a confirmed diagnosis of ITP, according to American Society of Hematology guidelines,16 for ≥3 months (persistent and chronic ITP) prior to randomization;
had a PC within 96 hours of randomization of either <30 × 109/L if they were not receiving steroid therapy or <50×109/L if receiving a stable dose of steroids for ≥2 weeks prior to screening; and
had failed to respond or relapsed after responding to 1 prior ITP therapy. Splenectomized subjects were eligible if their splenectomy had been performed more than 4 weeks prior to randomization.
Other key eligibility criteria included adequate renal (creatinine ≤1.5 times the upper limit of normal [×ULN]) and hepatic (total bilirubin, aspartate aminotransferase [AST], and alanine aminotransferase [ALT] all ≤3 ×ULN) function and no history of cardiovascular disease, thromboembolic disease, deep vein thrombosis (DVT), or any medical condition where systemic anticoagulation was required for >6 months. Subjects with a history of lupus anticoagulant or antiphospholipid syndrome were not eligible. In addition, all female subjects who were pregnant and/or lactating were excluded.
Treatment interventions and efficacy assessments
In the randomized study, subjects were assigned to once-daily oral avatrombopag (2.5, 5, 10, or 20 mg) or placebo in a ratio of 3:3:3:3:1, respectively, for 28 days or until withdrawal from the study. Dosing was done under fasting conditions, because food effect studies had not been performed at the time of the study execution; subsequent healthy volunteer studies have demonstrated that avatrombopag systemic exposures are not substantially altered when administered with food. Key study withdrawal criteria included administration of rescue medication for ITP, a PC increase to ≥500 × 109/L, and presence of a severe (grade 3 or 4) and/or serious adverse event (AE) related to the study drug.
In the 4-week randomized study, the primary efficacy end point was PC response rate, defined as the proportion of subjects who achieved PC ≥50 × 109/L and minimum PC increase of 20 × 109/L above baseline at day 28. Other efficacy end points included changes in median and mean PC, proportion of subjects who achieved PC ≥50 × 109/L and ≥100 × 109/L on day 28, and proportion of subjects who doubled their PC from baseline to day 28.
In the extension study, responders at day 28 continued on a fixed blinded regimen, taking their same daily dose of avatrombopag (or placebo) in the extension study. Nonresponders at day 28 in the randomized study were given open-label avatrombopag 10 mg once daily when they entered the extension study; increases up to 40 mg once daily were permitted as needed to maintain a PC >50 × 109/L. Reductions in concomitant ITP medications were not permitted in the randomized study but were permitted in the extension study. Dose reductions of up to 50% in concomitant ITP medications were permitted if PCs were >200 × 109/L; further reductions were permitted at 2-week intervals if increased PCs were sustained.
The primary objectives of the extension study were to assess the safety and tolerability of avatrombopag for an additional 24 weeks. Secondary objectives assessed markers of effectiveness such as change in PC, maintenance of PC, and decrease in concomitant ITP medications. After 18 subjects had enrolled in the extension study, the protocol was amended to allow more flexible, open-label dose escalation in 10-mg increments every 14 days to a maximum of 40 mg, depending on the subject’s PC. Responders were held to a maximum of the blinded dose of study drug plus 20 mg/day of avatrombopag, whereas nonresponders could escalate their dose up to a maximum of 40 mg/day, providing individualized dosing based on response to treatment. If an excessive PC (≥500 × 109/L) occurred, the dosing was stopped and the PC monitored weekly until it decreased to ≤200 × 109/L. Dosing was then restarted at 1 dose level lower.
The extension study assessed the proportion of study participants who achieved a durable response. This was defined as subjects who had PC responses at ≥75% of their PC assessments over the last 14 weeks of the study and had a minimum of 3 PC measurements; if a subject had only 3 visits with PC measurements, all 3 measurements were required to be classified as a PC response for the response to be counted as durable. Per protocol, PC values were measured biweekly through week 24. Subjects who did not meet the minimum PC measurements and those using rescue medication or needing splenectomy by definition could not have a durable response. In addition, the proportion of subjects achieving an overall response was also assessed. An overall response was defined as a durable response or a transient PC response (which was PC responses at ≥2 consecutive study visits at any time during the extension study). Subgroup analyses of durable response included baseline PC category (≤15 × 109/L vs >15 × 109/L) and history of splenectomy.
At the end of the extension, the study drug was discontinued, followed by a 4-week follow-up period during which the PC was determined twice weekly (weeks 1 and 2) and then once weekly (weeks 3 and 4).
Safety assessments
Continuous monitoring of AEs was performed. The severity of an AE was graded by the investigator using the Common Terminology Criteria for Adverse Events v3.0. Laboratory evaluations (PC, hematology, coagulation, serum chemistry, urinalysis, and electrocardiograms) and clinical assessments, including medical history, vital signs, and concomitant medications, were recorded at intervals during the study period. Splenic ultrasound was performed periodically during the extension study. Bleeding was reported using Common Terminology Criteria for Adverse Events v3.0, under the category of hemorrhage/bleeding, and the time to the first bleeding event was performed as an exploratory analysis.
Statistical analyses
Because this was a proof-of-concept study, it was not powered to detect statistically significant changes in efficacy outcomes. No formal inferential testing was planned, and no adjustment for multiplicity was performed; all P values that have been reported are nominal. All analyses presented were prespecified.
Primary efficacy analyses were conducted in the intent-to-treat group that included all randomized subjects who had at least 1 postbaseline PC. Primary and secondary efficacy variables were examined by response rate based on the number and percentage of subjects and summarized by treatment group using last observation carried forward. An exploratory pairwise analysis of the primary efficacy variable was performed using Fisher’s exact test (for each pair of treatment groups; 10 comparisons in total). Analyses of safety included all subjects who received at least 1 dose of study drug and had at least 1 postbaseline safety assessment.
Results
Subject population
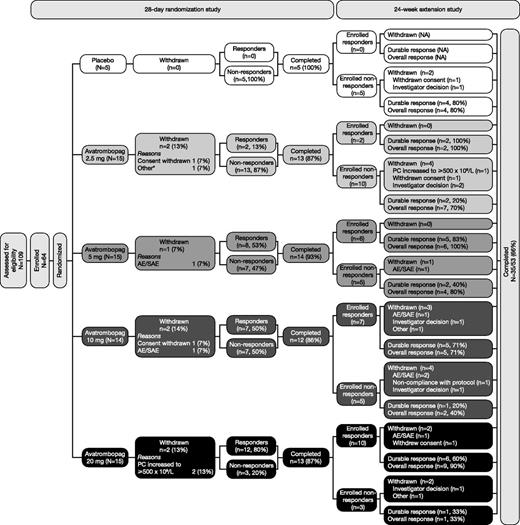
Subject demographic and baseline characteristics were generally comparable across the study groups (Table 1). Sixty-four subjects received treatment in the randomized study, and 53 subjects (83%) continued into the extension study. Subject flow throughout the randomized and extension studies is shown in Figure 1. Results from each of the randomized and extension studies are described below; a summary of the key efficacy end points throughout both studies is included in Figure 1 for reference.
Baseline demographics and subject characteristics by treatment group and study
| Category . | Randomized study . | Extension study . | ||||
|---|---|---|---|---|---|---|
| Avatrombopag . | Placebo (n= 5) . | |||||
| 2.5 mg (n = 15) . | 5 mg (n = 15) . | 10 mg (n = 14) . | 20 mg (n = 15) . | All avatrombopag doses (n = 53) . | ||
| Mean (SD) age, y | 53 (18) | 56 (18) | 58 (18) | 48 (17) | 40 (21) | 50 (18) |
| Male, n (%) | 6 (40) | 6 (40) | 6 (43) | 4 (27) | 2 (40) | 15 (28) |
| Race, n (%) | ||||||
| Asian | 1 (7) | 2 (13) | 0 | 1 (7) | 0 | 1 (2) |
| African American | 2 (13) | 0 | 1 (7) | 2 (13) | 0 | 5 (9) |
| Hispanic | 1 (7) | 1 (7) | 1 (7) | 1 (7) | 1 (20) | 5 (9) |
| White | 11 (73) | 11 (73) | 12 (86) | 10 (67) | 4 (80) | 40 (76) |
| Other | 0 | 1 (7) | 0 | 1 (7) | 0 | 2 (4) |
| Baseline steroid use: yes, n (%) | 4 (27) | 8 (53) | 6 (43) | 10 (67) | 3 (60) | 25 (47) |
| Baseline PC ≤15 × 109/L, n (%) | 5 (33) | 2 (13) | 5 (36) | 4 (27) | 2 (40) | 15 (28) |
| History of splenectomy: yes, n (%) | 5 (33) | 4 (27) | 3 (21) | 6 (40) | 2 (40) | 17 (32) |
| Category . | Randomized study . | Extension study . | ||||
|---|---|---|---|---|---|---|
| Avatrombopag . | Placebo (n= 5) . | |||||
| 2.5 mg (n = 15) . | 5 mg (n = 15) . | 10 mg (n = 14) . | 20 mg (n = 15) . | All avatrombopag doses (n = 53) . | ||
| Mean (SD) age, y | 53 (18) | 56 (18) | 58 (18) | 48 (17) | 40 (21) | 50 (18) |
| Male, n (%) | 6 (40) | 6 (40) | 6 (43) | 4 (27) | 2 (40) | 15 (28) |
| Race, n (%) | ||||||
| Asian | 1 (7) | 2 (13) | 0 | 1 (7) | 0 | 1 (2) |
| African American | 2 (13) | 0 | 1 (7) | 2 (13) | 0 | 5 (9) |
| Hispanic | 1 (7) | 1 (7) | 1 (7) | 1 (7) | 1 (20) | 5 (9) |
| White | 11 (73) | 11 (73) | 12 (86) | 10 (67) | 4 (80) | 40 (76) |
| Other | 0 | 1 (7) | 0 | 1 (7) | 0 | 2 (4) |
| Baseline steroid use: yes, n (%) | 4 (27) | 8 (53) | 6 (43) | 10 (67) | 3 (60) | 25 (47) |
| Baseline PC ≤15 × 109/L, n (%) | 5 (33) | 2 (13) | 5 (36) | 4 (27) | 2 (40) | 15 (28) |
| History of splenectomy: yes, n (%) | 5 (33) | 4 (27) | 3 (21) | 6 (40) | 2 (40) | 17 (32) |
Baseline was defined as the last observation (within 4 days) before the start of study drug in the randomized study.
SD, standard deviation.
Flow diagram of subject disposition and response rates for the avatrombopag double-blind and extension studies. *Continued grade 3 or 4 thrombocytopenia (lack of efficacy); responders indicates those subjects with a PC response of ≥50 × 109/L with ≥20 × 109/L increase above baseline at day 28; durable response indicates PC response at ≥75% of their platelet assessments over the last 14 weeks; overall response indicates stable response or response at any ≥2 consecutive visits. In total, there were 28 (53%) and 40 (76%) subjects with durable and overall responses, respectively. SAE, serious adverse event.
Flow diagram of subject disposition and response rates for the avatrombopag double-blind and extension studies. *Continued grade 3 or 4 thrombocytopenia (lack of efficacy); responders indicates those subjects with a PC response of ≥50 × 109/L with ≥20 × 109/L increase above baseline at day 28; durable response indicates PC response at ≥75% of their platelet assessments over the last 14 weeks; overall response indicates stable response or response at any ≥2 consecutive visits. In total, there were 28 (53%) and 40 (76%) subjects with durable and overall responses, respectively. SAE, serious adverse event.
Efficacy
Randomized study.
A higher proportion of subjects achieved a PC response in all avatrombopag dose groups than in the placebo group. At day 28, the response rates were 13%, 53%, 50%, and 80%, respectively, in the avatrombopag 2.5-, 5-, 10-, and 20-mg groups compared with 0% in the placebo group. Most responses to avatrombopag occurred by day 7 (Figure 2A). A clear dose response with regard to median PC over time was observed (Figure 2B); however, there was a notable decreased median PC over time from day 14 to day 28 in the 20-mg group.
Response rate for avatrombopag and placebo cohorts and median [Q1, Q3] PC over time by treatment group in the randomized study. Response rate (proportion of subjects who achieved PC ≥50 × 109/L and minimum PC increase of 20 × 109/L above baseline) at each time point for avatrombopag and placebo cohorts (A) and median [Q1, Q3] platelet count over time by treatment group (B) in the randomized study (LOCF). For each median (second quartile) PC presented in panel B, error bars denote the first (lower value of bar) and third (upper value of bar) quartiles. LOCF, last observation carried forward.
Response rate for avatrombopag and placebo cohorts and median [Q1, Q3] PC over time by treatment group in the randomized study. Response rate (proportion of subjects who achieved PC ≥50 × 109/L and minimum PC increase of 20 × 109/L above baseline) at each time point for avatrombopag and placebo cohorts (A) and median [Q1, Q3] platelet count over time by treatment group (B) in the randomized study (LOCF). For each median (second quartile) PC presented in panel B, error bars denote the first (lower value of bar) and third (upper value of bar) quartiles. LOCF, last observation carried forward.
Treatment with avatrombopag 20 mg/day resulted in a significantly greater proportion of responses (80%) compared with placebo (0%; P = .0036). A dose-dependent relationship was evident for median PC in the secondary end point analyses, with the largest PC increases occurring in the avatrombopag 20-mg dose group (Figure 2B). Avatrombopag 20 mg also resulted in a significantly higher proportion of subjects doubling their PC compared with placebo (87% vs 20%; P = .0139). Eighteen subjects (30.5%) treated with avatrombopag achieved a PC ≥100 × 109/L on day 28; 8 of these (53.3% of the group; P = .0547 vs placebo) were in the 20-mg group. No subjects in the placebo group achieved a PC ≥100 × 109/L. The proportion of subjects with a PC ≥100 × 109/L on day 28 in the 20-mg group (8/15 or 53%) was significantly higher than that in the 2.5-mg group (1/15 or 6.7%; P = .0142).
Extension study.
Of the 53 subjects enrolled in the extension study (Figure 1), 25 were responders and 28 were nonresponders in the randomized study. In the extension study, 40 out of 53 subjects (76%) and 28 out of 53 subjects (53%) achieved an overall response and durable response, respectively.
Over the extension study period, median PC across all subjects increased from 22 × 109/L at baseline to 56 × 109/L at week 4 (n = 51) and to 112.5 × 109/L at week 24 (n = 38) (Figure 3). Most responders in the 4-week randomized study (18/25 or 72%) achieved a durable response in the extension study. In contrast, among nonresponders in the randomized study, only 10 out of 28 (36%) achieved a durable response in the extension study.
Median [Q1, Q3] PC over time across all subjects in the extension study and during the 4-week follow-up period (observed data). For each median (second quartile) PC, error bars denote the first (lower value of bar) and third (upper value of bar) quartiles. FL, follow-up period after avatrombopag treatment period.
Median [Q1, Q3] PC over time across all subjects in the extension study and during the 4-week follow-up period (observed data). For each median (second quartile) PC, error bars denote the first (lower value of bar) and third (upper value of bar) quartiles. FL, follow-up period after avatrombopag treatment period.
Exploratory subgroup analyses found higher rates of durable response among those with baseline PC >15 × 109/L (vs ≤15 × 109/L) or with no history of splenectomy (Figure 4).
Proportion of subjects with a durable response (PC response at ≥75% of a minimum of 3 PC assessment visits occurring in the last 14 weeks of the extension study), stratified by baseline PC and splenectomy status in the extension study (observed data). *Avatrombopag responders in the extension study. Shown are the proportions of all avatrombopag-treated subjects with response-level PC (full analysis population).
Proportion of subjects with a durable response (PC response at ≥75% of a minimum of 3 PC assessment visits occurring in the last 14 weeks of the extension study), stratified by baseline PC and splenectomy status in the extension study (observed data). *Avatrombopag responders in the extension study. Shown are the proportions of all avatrombopag-treated subjects with response-level PC (full analysis population).
Twenty-four subjects were using steroids at extension study entry, of whom 13 had a ≥50% reduction in steroid dose and 8 permanently discontinued concomitant steroid medication (no steroid use during the last 8 weeks of the extension study).
A Kaplan-Meier plot of the time to the first bleeding event for the randomized and extension studies performed as an exploratory analysis demonstrated a decrease in the proportion of subjects with bleeds by week 14 (see supplemental Figure 1, available on the Blood Web site).
Dose and dose adjustment in the extension study
Overall, the mean and median final doses of avatrombopag at the end of the extension study were 15 mg and 10 mg, respectively. Only 5 of 25 responders (20%) from the randomized study required upward dose titration in the extension study compared with 21 (75%) of the 28 nonresponders.
Safety
Adverse events.
The most common AEs occurring in >10% of subjects across both studies (fatigue, headache, epistaxis, and contusion) are shown in Table 2. No deaths were reported during the studies. An overall safety profile of avatrombopag during the combined studies is presented in Table 3.
Summary of safety and most common AEs (occurring in more than 10% of subjects in the combined avatrombopag treatment groups) during the randomized and extension studies
| AE . | Total number of subjects receiving avatrombopag (N = 64) . | ||
|---|---|---|---|
| Any AE* . | Severe AE† . | Serious AE . | |
| No. of subjects with ≥1 AE | 64 (100) | 26 (41) | 12 (19) |
| Fatigue | 24 (38) | 2 (3) | 0 |
| Headache | 21 (33) | 1 (2) | 0 |
| Epistaxis | 16 (25) | 1 (2) | 0 |
| Contusion | 13 (20) | 0 | 0 |
| Arthralgia | 9 (14) | 0 | 0 |
| Diarrhea | 9 (14) | 1 (2) | 1 (2) |
| Severe thrombocytopenia (platelets <10 × 109/L) | 9 (14) | 8 (13) | 5 (8) |
| Gingival bleeding | 8 (13) | 0 | 0 |
| Back pain | 7 (11) | 1 (2) | 1 (2) |
| Peripheral edema | 7 (11) | 1 (2) | 0 |
| Petechiae | 7 (11) | 0 | 0 |
| PC increased | 7 (11) | 7 (11) | 0 |
| Vomiting | 7 (11) | 2 (3) | 2 (3) |
| AE . | Total number of subjects receiving avatrombopag (N = 64) . | ||
|---|---|---|---|
| Any AE* . | Severe AE† . | Serious AE . | |
| No. of subjects with ≥1 AE | 64 (100) | 26 (41) | 12 (19) |
| Fatigue | 24 (38) | 2 (3) | 0 |
| Headache | 21 (33) | 1 (2) | 0 |
| Epistaxis | 16 (25) | 1 (2) | 0 |
| Contusion | 13 (20) | 0 | 0 |
| Arthralgia | 9 (14) | 0 | 0 |
| Diarrhea | 9 (14) | 1 (2) | 1 (2) |
| Severe thrombocytopenia (platelets <10 × 109/L) | 9 (14) | 8 (13) | 5 (8) |
| Gingival bleeding | 8 (13) | 0 | 0 |
| Back pain | 7 (11) | 1 (2) | 1 (2) |
| Peripheral edema | 7 (11) | 1 (2) | 0 |
| Petechiae | 7 (11) | 0 | 0 |
| PC increased | 7 (11) | 7 (11) | 0 |
| Vomiting | 7 (11) | 2 (3) | 2 (3) |
Data represent number (%) of subjects.
Any grade or relationship.
Grade 3 or 4.
Overall safety profile of avatrombopag during the randomized and extension studies
| AE category* . | Total number of subjects receiving avatrombopag (N = 64) . |
|---|---|
| ≥1 AE during treatment | 64 (100) |
| Severe (grade 3-4) AEs | 26 (41) |
| Suspected drug-related AEs† | 42 (66) |
| Serious AEs | 12 (19) |
| Serious treatment-related AEs | 4 (6) |
| Withdrawal of study drug due to AE | 10 (16) |
| Dose interruption due to AE | 8 (13) |
| Deaths | 0 |
| AE category* . | Total number of subjects receiving avatrombopag (N = 64) . |
|---|---|
| ≥1 AE during treatment | 64 (100) |
| Severe (grade 3-4) AEs | 26 (41) |
| Suspected drug-related AEs† | 42 (66) |
| Serious AEs | 12 (19) |
| Serious treatment-related AEs | 4 (6) |
| Withdrawal of study drug due to AE | 10 (16) |
| Dose interruption due to AE | 8 (13) |
| Deaths | 0 |
Data represent number (%) of subjects.
Subjects may fall into >1 category.
Related AEs include those whose relationship was categorized as possible or probable by the investigator.
In the randomized study, the most frequently reported AEs (in ≥10% of subjects who received avatrombopag) were fatigue, headache, and epistaxis; these occurred at a similar rate to placebo. The only dose-related AE observed in the randomized study was increased PC, reported in 4 subjects receiving 20 mg (supplemental Table 1). Two of these subjects had PC >500 × 109/L and had to be permanently discontinued from the study. Seven subjects had reported AEs of increased PC across the combined studies; 5 of these 7 subjects had treatment permanently discontinued.
Six percent of subjects (n = 4/63) reported 5 thromboembolic events. The reported thromboembolic events (and associated PCs around the time of the events) were iliac DVT (19 × 109/L), stroke (119 × 109/L), superficial thrombophlebitis (571 × 109/L), myocardial infarction (MI) (47 × 109/L), and retinal artery occlusion (27 × 109/L). The retinal artery occlusion was reported in the same subject who reported the MI, 14 days after that subject discontinued study drug. Two of the thromboembolic AEs (iliac DVT and MI) resulted in permanent discontinuation of the subject from the study. The subject with the report of stroke underwent a temporary withdrawal of study drug. Three of 4 subjects with reported thromboembolic events had other risk factors for thrombosis; for example, the subject who reported the MI and retinal artery occlusion had a significant cardiovascular history of transient ischemic attacks, MIs, coronary artery bypass graft, and angioplasty (his/her inclusion was a protocol violation).
In this study, recurrence of severe thrombocytopenia was defined as PC that dropped below 10 × 109/L upon discontinuation of avatrombopag. This occurred in 14% (n = 9/64) of subjects in the follow-up period; all had received avatrombopag doses ≥10 mg. These recurrences occurred in 11% (n = 1/9) at 1 week, 56% (n = 5/9) at 2 weeks, 22% (n = 2/9) at 3 weeks, and 11% (n = 1/9) at 4 weeks after discontinuation of avatrombopag dosing. Six of these 9 subjects had PC below 10 × 109/L and 10 × 109/L less than baseline upon discontinuation of avatrombopag, which is the definition of recurrence of severe thrombocytopenia used in other TPO-RA studies.17
Bleeding AEs were reported in 67% (n = 43/64) of subjects, of which the majority (90%) were grade 1 or 2 (ie, mild to moderate). Only 6.3% (n = 4/64) of subjects reported grade 3 or 4 bleeds. The reported grade 3 or 4 bleeding events (reported as Preferred Terms, MedDRA v10.1) were grade 4 gastrointestinal (gastric) bleed (PC of 2 × 109/L), grade 3 intracranial bleed (2 × 109/L), grade 3 hemorrhagic diathesis (reported as increased bleeding by the investigator) (4 × 109/L), and grade 3 epistaxis (PC was 98 × 109/L 12 days after bleed).
Avatrombopag did not have an adverse effect on renal function, nor was it associated with clinically relevant changes in coagulation. Fifteen of the 21 grade 3 or 4 laboratory abnormalities that occurred across the combined randomized and extension studies were related to PC: thrombocytopenia <10 × 109/L in 8 subjects and increased PC in 7 subjects. Splenic ultrasound in the extension study identified only 2 investigator-assessed clinically relevant findings (splenomegaly and hyperechoic lesion). There were 2 events of grade 2 or 3 in increased liver function tests (1 ALT and 1 AST) in subjects receiving avatrombopag. There were no reports of ALT or AST >3 ×ULN or significant risk factors for drug-induced liver injury (as demonstrated by Hy’s law cases; ie, >3 ×ULN elevated aminotransferases with elevated total bilirubin and without initial findings of cholestasis [serum alkaline phosphatase activity >2 × ULN]). Transient changes were observed for liver function tests and other laboratory parameters, but no dose-related trends were observed except for the aforementioned PC on treatment and decreased PC after discontinuing treatment. No clinically relevant changes in vital signs, physical examination findings, or electrocardiographic parameters occurred in the combined analyses.
The incidence of severe (grade 3 or 4) AEs is presented in supplemental Table 2.
Treatment discontinuation.
Interruption of study-drug treatment (temporary treatment discontinuation) as a result of an AE occurred in 8 subjects (13%) across both studies (Table 3). Five of these subjects had a dose interruption due to increased PC. The 3 remaining subjects had a dose interruption due to grade 2 elevated ALT (n = 1), grade 2 leukocytosis (n = 1), and grade 3 cerebrovascular accident (n = 1).
Permanent treatment discontinuation as a result of an AE occurred in a combined total of 16% (n = 10/63) of subjects (4 in the randomized study and 6 in the extension study; Table 3). Across studies, increased PC was the only AE that led to permanent treatment discontinuation in >1 subject (occurring in 2 in the randomized study and 3 in the extension study). One subject, receiving avatrombopag 10 mg in both the randomized and extension studies, permanently discontinued treatment due to grade 2 leukocytosis that occurred during the extension study. Further evaluation resulted in diagnosis of myelodysplastic syndrome (MDS; refractory anemia with excess blasts type), and the subject was discontinued from the study. Approximately 1 month later, grade 4 acute myelogenous leukemia (French-American-British classification M2) developed. There was 1 discontinuation due to grade 2 musculoskeletal chest pain.
Discussion
The phase 2 randomized and open-label extension studies support further study of once-daily oral avatrombopag in subjects with ITP. Over the 28-day randomized study period, dose-dependent response rates were observed with avatrombopag (see Figures 2 and 3). Significantly more subjects responded to avatrombopag 20 mg compared with placebo. Fifty-three patients entered the extension study, and the response rate was higher than in the randomized study because of the ability to increase the doses.
Of note in the randomized study is that there was an observed decrease in median PC over time from day 14 to day 28 in the 20-mg group (randomized study; see Figure 2B). A sensitivity analysis removing those subjects who underwent discontinuations due to increased PC at day 14 (n = 2) demonstrated that there was still a discernible decrease in median PC from day 14 to day 28 in this group. Despite this apparent drop in median PC, the overall response rates at day 14 and day 28 in the 20-mg group (93% and 80%) were broadly comparable.
Over the course of the 24-week extension study, 53% of subjects achieved a durable response; the durable platelet response end point used in this study was slightly different from durable end points used in other TPO-RA trials.17,18 In the extension study, PC measurements were taken every second week, as opposed to weekly, over a 14-week period. The durable end point suggests the ability of avatrombopag to achieve and maintain clinically relevant PC increases. Subgroup analyses demonstrated that there were more durable responses in those subjects who had not undergone a splenectomy or who had baseline PC >15 × 109/L. The lower response in splenectomized subjects might simply reflect that this is a more refractory group of subjects. Caution should be used when interpreting these subgroup analyses, because the sample sizes were very small.
A total of 10 out of 28 (36%) nonresponders in the randomized study had a durable response in the extension study. Subjects had an opportunity either to receive avatrombopag dosing (previous placebo subjects) or to undergo dose adjustment and receive higher-dose avatrombopag.
Treatment with avatrombopag was generally well tolerated; low rates of severe AEs, serious AEs, and study drug discontinuations due to AEs were observed. Overall, the AE profile was comparable with those reported in previous trials of TPO-RAs; for example, in rates of thromboembolic events or recurrence of thrombocytopenia.
As expected, due to the mechanism of action of TPO-RAs, recurrence of severe thrombocytopenia developed upon discontinuation of avatrombopag in 14% of subjects. The recurrence of severe thrombocytopenia on discontinuation of avatrombopag appeared to be dose dependent, because all 9 subjects were in the higher (10-mg and 20-mg) dose groups. Tapering of the dose has been suggested as a possible method to reduce the occurrence of severe thrombocytopenia but was not explored in this study.10
The bleeding AEs were primarily of mild to moderate severity. The bleeding resolved in all 4 subjects who reported a grade 3 or 4 bleed. The frequency of bleeding events diminished over the course of treatment, with the majority of events occurring by week 14. At this time point, subjects would have had the opportunity to dose adjust to optimize their PC response.
The frequency of thromboembolic events in the long-term studies of romiplostim and eltrombopag (6% for each)19,20 is similar to the thromboembolic event rates seen in these studies (6.3%). As in the published data, the majority of subjects (ie, 75%, n = 3/4) had risk factors for thromboembolic events. No trend was noted between elevated PCs and thromboembolic events in any of these studies.
One subject developed grade 3 leukocytosis progressing to MDS and then acute myelogenous leukemia. It is likely that this subject did not have ITP at study entry but rather an underlying MDS. Potentially, avatrombopag dosing may have stimulated an increase in blast cells in this subject. This subject’s experience suggests that bone marrow analysis early on might be prudent in cases where any suspicion of MDS exists.
Two subjects in the extension study had splenic ultrasound findings. One subject had a small change in splenic length from 10.5 cm to 12.0 cm. This subject’s AE profile and laboratory assessments revealed no other hematologic disease during the study. The second subject had a 1.5-cm hyperechoic splenic lesion thought likely to represent a splenic hemangioma that remained unchanged throughout the extension study.
The primary limitation was that the current studies were not powered to derive unequivocal conclusions with a sample size of only 64 subjects, of whom only 5 were in the placebo group. However, this was deemed an adequate sample size to determine a treatment effect while minimizing the number of subjects exposed to placebo. The small sample size limits the conclusions that can be drawn.
Further limitations pertain to the large intersubject variability for PC (for example, as seen in Figure 3), compounded by the comparatively few dose discontinuations and interruptions.
Additional experience with avatrombopag in a wider subject population will also provide further information on any food effects that may occur, such as those seen in subjects taking eltrombopag.10 In addition, although mild derangement of hepatic enzymes was observed in this study, no severe hepatic toxicity associated with avatrombopag was observed. Larger clinical studies are required to fully characterize avatrombopag’s hepatic safety profile.
In summary, avatrombopag achieved increases in PCs, was relatively well tolerated, and had an acceptable safety profile in these 2 phase 2 studies of subjects with ITP. Significant PC responses were achieved vs placebo during the 28-day randomized study, and stable PC responses were observed over 6 months in the subsequent extension study. Based on these phase 2 data, avatrombopag is a candidate for further study and development in the treatment of ITP.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the study investigators, coordinators, nurses, and subjects and their families for their invaluable contributions to this study. The authors also thank David Squillacote for critical review of the manuscript.
This study was sponsored by Eisai. Editorial support was provided by Michael G. Pellegrino and Gary Dever of Complete Medical Communications and was funded by Eisai.
Authorship
Contribution: All authors analyzed and interpreted the data, contributed toward critical revision of the manuscript, and approved the final draft; J.B.B. and J.M. led the development and writing of the initial draft of the manuscript and provided ongoing comments on the writing; D.J.K. provided substantial input and critical direction to the initial draft of the manuscript; J.M. provided additional clinical information; S.T. performed statistical analyses; and J.B.B. had final responsibility for the decision to submit for publication.
Conflict-of-interest disclosure: J.B.B. received research support from Amgen, Cangene, GlaxoSmithKline, Genzyme, IgG of America, Immunomedics, Ligand, Eisai, Shionogi, and Sysmex. J.B.B.’s family owns stock in Amgen and GlaxoSmithKline. J.B.B. has participated in advisory boards for Amgen, GlaxoSmithKline, Ligand, Shionogi, Symphogen, and Eisai; D.J.K. received research support from Eisai, ONO, and Pfizer and is a consultant for Amgen and GlaxoSmithKline; L.M.A. received research support from Eisai and is on the Amgen speakers’ bureau; C.M.K. received research support from Eisai and Grifols and is a consultant for Amgen; A.C. received research support from Eisai and Stago and is a consultant for Baxter, Bayer, Daiichi-Sankyo, and Genzyme; K.B.P. received research support from Eisai; and S.T. and J.M. are employees of Eisai.
Correspondence: James B. Bussel, Division of Hematology/Oncology, Department of Pediatrics and Medicine, New York Presbyterian Hospital, Weill Medical College of Cornell University, 525 East 68th St, Payson 695, New York, NY 10021; e-mail: jbussel@med.cornell.edu.

![Figure 2. Response rate for avatrombopag and placebo cohorts and median [Q1, Q3] PC over time by treatment group in the randomized study. Response rate (proportion of subjects who achieved PC ≥50 × 109/L and minimum PC increase of 20 × 109/L above baseline) at each time point for avatrombopag and placebo cohorts (A) and median [Q1, Q3] platelet count over time by treatment group (B) in the randomized study (LOCF). For each median (second quartile) PC presented in panel B, error bars denote the first (lower value of bar) and third (upper value of bar) quartiles. LOCF, last observation carried forward.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/123/25/10.1182_blood-2013-07-514398/4/m_3887f2.jpeg?Expires=1769084558&Signature=uxBPpFbCAsvnDsnGah7N7IVqHFMFpODc8nBeyUdmAsvMLgYTAaj7bbFv8kVv59de4OnixIfOc~j77z7Fe5jG5gCen7OCH5kNAeJE~PUpYe4sRlKK3m9qFKM5X0nujsmXQiXSjLYBbnNYmyuMMDKrn9hFpUjCBtrxEIRSdOKYTXrSkPlg6nXuej1CaUwsW~5gbnajPNf253PCsHU5Pl0trpLdgE4u7ynGy0hrxzlOyz7win8Qrrlx9r-sYKMztVXuMCN0tUsuTPilN2mhSpQcfY-LjJ8fqAoHLQV5-oBPvTyJ3US4WYoLyHuQQ6r7ziRUCjcWvCFohQaaktoMhiZiEg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 3. Median [Q1, Q3] PC over time across all subjects in the extension study and during the 4-week follow-up period (observed data). For each median (second quartile) PC, error bars denote the first (lower value of bar) and third (upper value of bar) quartiles. FL, follow-up period after avatrombopag treatment period.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/123/25/10.1182_blood-2013-07-514398/4/m_3887f3.jpeg?Expires=1769084558&Signature=YeFqa8RauEBtmckKr~8nYlJdKtUfD6SnJ3lzhsd4dxr8lB7ptvvfh3sncwZSzLNeSCW3IGt7EmEm4EBvz3ex~ntYmNDQW2hWSLVMVMHD7jQ3lykFTZW35I7OnVCzNJxkEKlNmmqbhy3SoJrNs96lz-1eQEA2PH029Qk02PMPF9SnEtRoeA~yTQlH4woBvnSDjnzPc0QLnI2Yu4MSJxHh02tqGOg3QRQ3a2SHrz2tOyExFcLc~ej1TfGwWa1j~8phYrR0WEKWASvGbs76w9707IyAdeSOKBkCO7HbtjZr2diJlHkqVjFw-nZQo3ZJ4Bo2Nlin5KQGV6wqeCSsqQu8DQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
