Key Points
Blockade of inhibitory KIRs with MHC class I antigens on lymphoma cells by anti-KIR antibodies augments NK-cell spontaneous cytotoxicity.
In combination with anti-CD20 mAbs, anti-KIR induces enhanced NK cell–mediated, rituximab-dependent cytotoxicity against lymphoma.
Abstract
Natural killer (NK) cells mediate antilymphoma activity by spontaneous cytotoxicity and antibody-dependent cell-mediated cytotoxicity (ADCC) when triggered by rituximab, an anti-CD20 monoclonal antibody (mAb) used to treat patients with B-cell lymphomas. The balance of inhibitory and activating signals determines the magnitude of the efficacy of NK cells by spontaneous cytotoxicity. Here, using a killer-cell immunoglobulin-like receptor (KIR) transgenic murine model, we show that blockade of the interface of inhibitory KIRs with major histocompatibility complex (MHC) class I antigens on lymphoma cells by anti-KIR antibodies prevents a tolerogenic interaction and augments NK-cell spontaneous cytotoxicity. In combination with anti-CD20 mAbs, anti-KIR treatment induces enhanced NK-cell–mediated, rituximab-dependent cytotoxicity against lymphoma in vitro and in vivo in KIR transgenic and syngeneic murine lymphoma models. These results support a therapeutic strategy of combination rituximab and KIR blockade through lirilumab, illustrating the potential efficacy of combining a tumor-targeting therapy with an NK-cell agonist, thus stimulating the postrituximab antilymphoma immune response.
Introduction
Immune checkpoint blockade represents a promising cancer therapy that aims to restore an efficient antitumoral response mediated by endogenous immune cells.1 Antibodies to CTLA-4, an inhibitory receptor that dampens T-cell receptor (TCR) signaling, enhance immune cell function by blocking a negative regulator. CTLA-4 shares CD80 (B7.1) and CD86 (B7.2) as ligands with the TCR costimulatory receptor CD28. The intracellular signals transduced by the TCR, CD28, and CTLA-4 determine the outcome of T-cell activation.2 The therapeutic concept of immunomodulation was validated by the approval of anti–CTLA-4 ipilimumab in metastatic melanoma, thus increasing overall survival.1,3 Other inhibitory receptors of T-cell function, such as PD-1 and LAG-3, are being targeted by therapeutic monoclonal antibodies (mAbs) in clinical and preclinical development.1,4,5
As a corollary to targeting negative regulators of T cells, we hypothesized that the killer cell immunoglobulin-like receptor (KIR) family of natural killer (NK) cell negative regulators would represent a novel and active class of immunotherapy.6 Indeed, NK cells play critical roles in host defense against infections and tumors by secreting immunoregulatory cytokines and by killing infected or transformed cells. The activation of NK-cell effector function is regulated by multiple types of activating and inhibitory receptors, including KIR, that recognize ligands expressed on potential target cells. The balance between positive and negative signals transmitted via these NK receptors determines whether or not a target cell is killed by an NK cell.7 In addition, lack of KIR-HLA class I interactions has been associated with potent NK-mediated antitumor efficacy and increased survival in acute myeloid leukemia (AML) patients upon haplo-identical stem cell transplantation from KIR mismatched donors.8 To exploit this pathway pharmacologically, the fully human mAb anti-KIR 1-7F9 (IPH2101) was first generated,9 and then a recombinant version of this mAb was developed with a stabilized hinge (lirilumab). 1-7F9 and lirilumab mAbs cross-react with KIR2DL1, -L2, and -L3 receptors and impair their inhibitory signaling by preventing their binding to HLA-C. In vitro, anti-KIR mAbs augmented NK-cell-mediated lysis of HLA-C-expressing tumor cells, including autologous AML blasts and autologous CD138+ multiple myeloma cells.9,10 In addition, splenocytes from major histocompatibility complex class I (MHC-I)–deficient mice expressing HLA-Cw3 were rejected in 20 hours from Rag1KO mice expressing KIR2DL3 with increasing doses of 1-7F9, demonstrating that in vivo blockade of KIR HLA class I interactions could mediate rejection of HLA-C–expressing cells.9,11 In mice, the Ly49 receptors have functions similar to human KIRs and bind to murine H-2 (MHC-I) molecules. We demonstrated a beneficial effect of blocking H-2-Ly49 interactions in vivo in combination with lenalidomide in rejecting MHC-I–positive tumor cells.10 A phase 1 clinical trial in elderly patients with AML was performed with an escalating-dose of 1-7F9. Results demonstrated that the 1-7F9 mAb injections were safe and could block KIR for long periods of time (more than 2 weeks at 1 and 3 mg/kg) with limited adverse effects.12
More than a decade prior to the approval of ipilimumab, a murine-human chimeric immunoglobulin G1 (IgG1) antibody against CD20 called rituximab was approved and has since become a standard treatment for patients with B-cell lymphomas. Although rituximab has multiple mechanisms of action, antibody-dependent cell-mediated cytotoxicity (ADCC) is of particular importance. Neutralizing antibodies that prevent the Fc-FcR-γ interaction abrogate the B-cell–depleting and antilymphoma activity in vitro13 and in vivo in murine models.14-16 In clinical practice, FcγRIIIA polymorphism with a higher affinity for IgG1 is associated with a higher response rate.17,18 Because the response rate to rituximab among patients with relapsed/refractory lymphoma may be approximately half that of patients previously untreated, we investigated whether NK-cell immunomodulation by combination of blockade of inhibitory KIR by lirilumab and stimulation via FcγRIII by rituximab could enhance antilymphoma efficacy in preclinical models.
Here we present results that support the monotherapy activity of lirilumab in a KIR2DL3 transgenic lymphoma model and of anti-Ly49C/I F(ab′)2 in a C57BL/6 syngeneic lymphoma model. In both models tested, combination of either of those with an anti-CD20 mAb significantly improves the antitumor efficacy of anti-CD20 mAb alone. These findings provide rationale for a clinical trial in lymphoma investigating this novel combination of an anti-KIR mAb to tilt the balance of inhibitory and stimulatory NK signals favoring spontaneous cytotoxicity and to further enhance the efficacy of rituximab by augmentation of ADCC.
Material and methods
Cell lines and mice
Human B-cell line LCL 721.221 was transduced with lentiviral particles encoding either HLA-Cw3 (221 HLA-Cw3) or enhanced green fluorescent protein (eGFP) as a control (221), from which sequences were cloned into TripdU3 EF1a plasmid. EL4 murine T lymphoma cells were transduced with human CD20 complementary DNA (EL4-huCD20). Both cell lines were cultured in RPMI-1640 medium (Invitrogen/Life Technologies) supplemented with 10% heat-inactivated fetal calf serum (HyClone Laboratories), 100 U/mL penicillin and 100 μg/mL streptomycin (both from Invitrogen/Life Technologies), 2 mM l-glutamine (Sigma-Aldrich), and 1 mM sodium pyruvate (Sigma-Aldrich), with the addition of 50 μM 2-mercaptoethanol (Sigma-Aldrich) for EL-4 only. Cells were grown in suspension culture at 37°C in 5% CO2.
Eight- to 10-week-old male and female Rag1KO Tg KIR2DL3 (Rag1KO-Tg KIR) mice were bred and maintained at Innate Pharma animal facilities in specific pathogen-free conditions. Rag1KO Tg KIR2DL3 mice on a C57BL/6 background were previously described.9 Eight- to 10-week-old female C57BL/6 mice were purchased from Charles River and were housed at the Laboratory Animal Facility at the Stanford University Medical Center. All experiments using Rag1KO-Tg KIR mice were approved by the Innate Pharma ethics committee in accordance with the European directive for animal experimentation. Experiments using C57BL/6 mice were approved by Stanford Laboratory Animal Care and were conducted in accordance with Stanford University Animal Facility and National Institutes of Health guidelines.
Therapeutic antibodies and reagents
Anti-KIR mAb is a fully human IgG4 anti-KIR2DL1, -L2, -L3, -S1, -S2 produced in the CHO cell line (lirilumab/IPH2102/BMS-986015).9 Anti-CD20 mAb is a chimeric human IgG1 (rituximab [MabThera]; Roche). Phycoerythrin-conjugated lirilumab was produced at Innate Pharma. F(ab′)2 fragments of anti-Ly49C/I (5E6) mAbs were provided by Innate Pharma. The CAT-13.6E12 hybridoma cell line was purchased from Deutsche Sammlung von Mikroorganismen und Zellkulturen. These cells were used to produce the anti-huCD20 CAT-13 IgG2a mAb. Irrelevant antibodies, with the same isotypes as lirilumab (hIgG4) and rituximab (chimeric IgG1), 5% normal mouse serum, and 4D11 (Ly49G2, a mAb against Ly49G2 specific for H2-Dd) were used as controls.
In vitro NK functional assays
To evaluate NK-cell cytotoxicity against EL4-huCD20, chromium release was performed as described.19 Percent lysis was determined after 4-hour cultures of purified NK cells at variable effector:target cell ratios with 51Cr-labeled lymphoma cells in media alone, or with anti-Ly49C/I (5E6; 10 µg/mL) alone, anti-CD20 mAb (CAT-13; 10 µg/mL) alone, or the combination of anti-Ly49C/I and anti-CD20 mAbs (both at 10 µg/mL). To evaluate NK-cell degranulation, CD107a mobilization was assayed as detailed previously.20 Cells were cultured for interferon-γ (IFN-γ) assessment by using conditions similar to those detailed above for assessment of cytotoxicity. Supernatant was analyzed for IFN-γ by enzyme-linked immunosorbent assay. In vitro assays were performed with 3 independent samples.
Tumor transplantation and antibody therapy
In tumoral challenge experiments, 0.5 × 106 EL4-huCD20 lymphoma tumor cells in 50 μL of phosphate-buffered saline were injected retro-orbitally into wild-type C57BL/6 mice. In 300 μL of phosphate-buffered saline, 107 221 cells were injected intravenously into Rag1KO-Tg KIR mice. Anti-CD20 mAbs (250 µg per injection) and 200 µg of F(ab′)2 fragments of anti-Ly49C/I were administered by intraperitoneal injections, whereas all human mAbs were administered by intravenous injection. Tumor growth (EL4-huCD20 tumor model) and survival (221 tumor model) were monitored for 90 to 150 days after tumoral challenge. Tumor growth was measured by caliper twice a week and expressed as length times width in square centimeters. Mice were euthanized when tumor size reached 4 cm2 or when tumor sites ulcerated.
Depletion of CD8 T cells, NK cells, and macrophages
Anti-CD8 mAb (hybridoma 2.43), anti-Asialo-GM1 mAb (Wako Chemicals), and liposomal clodronate (Weissman Laboratory, Stanford, CA) were used to deplete CD8 T-cell, NK-cell, and macrophage activity in vivo in C57BL/6 mice, respectively. Depleting anti-CD8 mAb (500 µg) and anti-Asialo-GM1 mAb (50 µL) were injected intraperitoneally on day −1, day 0 of tumor inoculation, and every 5 days thereafter for 4 weeks. Liposomal clodronate was injected retro-orbitally on day −2 at a dose of 200 µL, on day 0 of tumor inoculation, and every 4 days thereafter for 4 weeks at a dose of 100 µL. The depletion conditions were validated by flow cytometry of blood showing more than 95% depletion of CD8 T cells, 90% depletion of NK cells, and 90% depletion of macrophages.
In Rag1KO-Tg KIR mice, NK-cell depletion was achieved by injecting 100 µg of anti-NK1.1 mAb (PK136) intravenously every 10 days, starting 1 day prior to treatment of 221 cells.
Antibodies for flow cytometry
The following mAbs to mouse antigens were used: CD8 fluorescein isothiocyanate (FITC) (Becton Dickinson [BD]/BD Biosciences (San Jose, CA), CD107a FITC (BD), CD4 FITC (BD), CD3 peridinin chlorophyll protein complex (BD), NK1.1 allophycocyanin (BD), and F4/80 allophycocyanin (eBioscience, San Diego, CA). Stained cells were collected on a FACSCalibur or an LSRII three-laser cytometer (BD), and data were analyzed by using Cytobank (http://www.cytobank.org).21
Statistical analysis
Prism software (GraphPad) was used to analyze tumor growth and luciferase light units and determine the statistical significance of differences between groups by applying an unpaired Student t test. Kaplan-Meier plots were used to analyze survival. Comparisons of survival curves were made by using the log-rank test. P values <.05 were considered significant. For tumor burdens, comparisons of means were done by analysis of variance.
Results
Anti-Ly49C/I F(ab′)2 increases anti-CD20 mAb-mediated NK-cell degranulation and cytotoxicity
To investigate the effects of blocking inhibitory receptors on NK cells in combination with a CD20-targeting antibody, we first selected a murine lymphoma cell line transfected with human CD20—EL4-huCD20—which was previously shown to be sensitive to anti-Ly49C/I mAb therapy.22 This model allowed targeting the murine homolog of the human KIR, the Ly49 family, using F(ab′)2 fragments of the anti-Ly49C/I mAb concurrently with an anti-CD20 mAb (CAT-13) therapy in an immune competent system. We first assessed whether blocking inhibitory NK-cell receptors by using anti-Ly49C/I F(ab′)2 could enhance anti-CD20–mediated NK-cell function, specifically degranulation and cytotoxicity. By using CD107a expression on murine NK cells as a marker of granule mobilization,23 we found that anti-CD20–induced degranulation could be significantly enhanced by anti-Ly49C/I F(ab′)2 (Figure 1A). IFNγ was also increased by anti-Ly49C/I F(ab′)2 (Figure 1B). We then assessed the effect of anti-Ly49C/I F(ab′)2 on anti-CD20–induced ADCC. Murine NK cells were purified and cultured with 51Cr-labeled EL4-huCD20 cells and anti-CD20 CAT-13 mAb in the presence or absence of anti-Ly49C/I F(ab′)2. The addition of anti-Ly49C/I F(ab′)2 significantly increased anti-CD20–induced ADCC compared with anti-CD20 CAT-13 mAb alone (Figure 1C).
Anti-Ly49C/I F(ab′)2increases anti-CD20 mAb-mediated NK-cell degranulation and cytotoxicity. (A) NK cells isolated and purified from C57BL/6 mice were analyzed for degranulation by CD107a mobilization after 24-hour culture with 5 conditions: medium alone; human CD20+ murine lymphoma cell line (EL4-huCD20) at a 1:1 ratio of tumor:NK cells; tumor and anti-CD20 mAb (CAT13; 10 µg/mL); tumor and anti-Ly49C/I F(ab′)2 (5E6; 10 µg/mL); or tumor, anti-CD20 mAb (10 µg/mL), and anti-Ly49C/I F(ab′)2 (10 µg/mL). *P = .0109. (B) Enzyme-linked immunosorbent assay (ELISA) results measuring IFN-γ following a 4-hour culture of purified murine NK cells in medium alone; EL4-huCD20 at a 1:1 ratio of tumor:NK cells; tumor and anti-CD20 mAb (CAT13; 10 µg/mL); tumor and anti-Ly49C/I F(ab′)2 (10 µg/mL); or tumor, anti-CD20 mAb (10 µg/mL), and anti-Ly49C/I F(ab′)2 (10 µg/mL). *P = .001. (C) Supernatant was harvested and analyzed by ELISA for IFN-γ. NK-cell cytotoxicity on EL4-huCD20 tumor cells was analyzed in a chromium-release assay. NK cells were purified before being incubated with 51Cr-labeled EL4-huCD20. (C) Percent lysis of target cells by chromium release at varying effector (purified murine NK cells):target (EL4-huCD20) cell ratios cultured with (●) medium alone, (▲) anti-Ly49C/I F(ab′)2 (10 µg/mL), (▼) anti-CD20 mAb (10 µg/mL), or (▪) the combination of both antibodies. *P = .019.
Anti-Ly49C/I F(ab′)2increases anti-CD20 mAb-mediated NK-cell degranulation and cytotoxicity. (A) NK cells isolated and purified from C57BL/6 mice were analyzed for degranulation by CD107a mobilization after 24-hour culture with 5 conditions: medium alone; human CD20+ murine lymphoma cell line (EL4-huCD20) at a 1:1 ratio of tumor:NK cells; tumor and anti-CD20 mAb (CAT13; 10 µg/mL); tumor and anti-Ly49C/I F(ab′)2 (5E6; 10 µg/mL); or tumor, anti-CD20 mAb (10 µg/mL), and anti-Ly49C/I F(ab′)2 (10 µg/mL). *P = .0109. (B) Enzyme-linked immunosorbent assay (ELISA) results measuring IFN-γ following a 4-hour culture of purified murine NK cells in medium alone; EL4-huCD20 at a 1:1 ratio of tumor:NK cells; tumor and anti-CD20 mAb (CAT13; 10 µg/mL); tumor and anti-Ly49C/I F(ab′)2 (10 µg/mL); or tumor, anti-CD20 mAb (10 µg/mL), and anti-Ly49C/I F(ab′)2 (10 µg/mL). *P = .001. (C) Supernatant was harvested and analyzed by ELISA for IFN-γ. NK-cell cytotoxicity on EL4-huCD20 tumor cells was analyzed in a chromium-release assay. NK cells were purified before being incubated with 51Cr-labeled EL4-huCD20. (C) Percent lysis of target cells by chromium release at varying effector (purified murine NK cells):target (EL4-huCD20) cell ratios cultured with (●) medium alone, (▲) anti-Ly49C/I F(ab′)2 (10 µg/mL), (▼) anti-CD20 mAb (10 µg/mL), or (▪) the combination of both antibodies. *P = .019.
Anti-Ly49C/I F(ab′)2 potentiates antilymphoma activity of anti-CD20 mAb in vivo
To test whether treatment with anti-Ly49C/I F(ab′)2 would enhance the antilymphoma activity of anti-CD20 mAb in vivo, we used a mouse lymphoma transfected with human CD20. Anti-Ly49C/I F(ab′)2 monotherapy has previously been shown to prolong survival against the murine lymphoma cell line EL4.22 Therefore, the EL4-huCD20 murine model provides an opportunity to test whether the combination of anti-Ly49C/I F(ab′)2 and anti-CD20 mAb elicits an enhanced efficacy in a therapeutic tumor model.
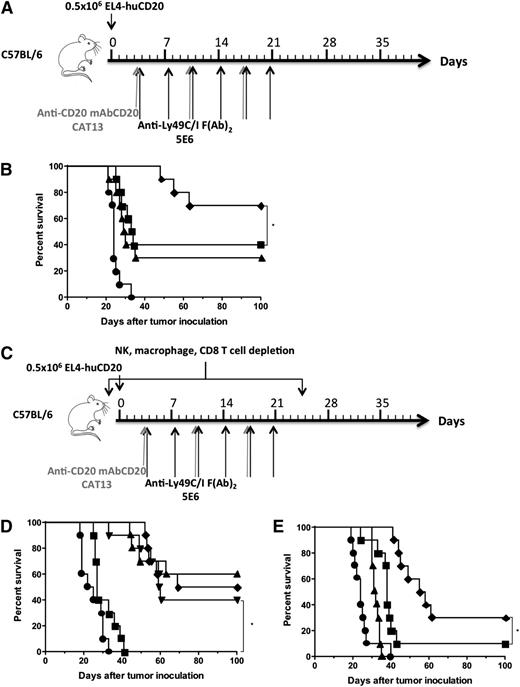
Although anti-CD20 mAb and anti-Ly49C/I F(ab′)2 both had antitumor activity when used as single agents, their combination significantly enhanced survival (Figure 2A-B). To determine activity against well-established tumors, therapy was delayed 1 week until day 10 resulting in decreased efficacy of both single agents and the combination. Anti-CD20 mAb and anti-Ly49C/I F(ab′)2 as monotherapy on day 10 minimally prolonged survival whereas combination of both on day 10 resulted in prolonged survival (Figure 2E).
Anti-Ly49C/I F(ab′)2enhances the antilymphoma activity of anti-CD20 mAb in vivo and is NK-cell–dependent. (A) C57BL/6 mice were inoculated retro-orbitally with 0.5 × 106 EL4-huCD20 lymphoma tumor cells. (B) After tumor inoculation, mice received (●) rat IgG control, (▪) 250 µg of anti-CD20 mAb (CAT-13) on day 3 and once per week for 3 weeks, (▲) 200 µg of anti-Ly49C/I F(ab′)2 (5E6) on day 3 and twice a week for 3 weeks, or (♦) the combination of both antibodies. Mice were then monitored for overall survival. *P = .042. (C) C57BL/6 mice were inoculated retro-orbitally with 0.5 × 106 EL4-huCD20 lymphoma tumor cells. (D) After tumor inoculation, mice received (●) rat IgG control on day 3; (▪) 50 µL of anti-Asialo-GM1 on days −1, 0, 5, 10, 15, 20, and 25 with 250 µg of anti-CD20 mAb and 200 µg anti-Ly49C/I F(ab′)2 on day 3; (▼) 200 µL liposomal clodronate on day −2 followed by 100 µL of liposomal clodronate on days 0, 4, 8, 12, 16, 20, and 24 with 250 µg of anti-CD20 mAb and 200 µg of anti-Ly49C/I F(ab′)2 on day 3; (♦) 500 µg anti-CD8 mAb on days −1, 0, 5, 10, 15, 20, and 25 with 250 µg of anti-CD20 mAb and 200 µg anti-Ly49C/I F(ab′)2 on day 3; or (▲) 250 µg of anti-CD20 mAb on day 3 and 200 µg of anti-Ly49C/I F(ab′)2 on day 3 with 250 µg of anti-CD20 mAb repeated once per week for 3 weeks and 200 µg of anti-Ly49C/I F(ab′)2 repeated biweekly for 3 weeks. Mice were then monitored for overall survival. *P < .001. All in vivo models were piloted with 5 mice per group and repeated with 10 mice per group. Isotype controls included 5% normal mouse serum and 250 µg of 4D11 (Ly49G2) on day 3 and biweekly for 3 weeks in addition to rat IgG with no effect on tumor growth or survival (representative control, rat IgG, shown). (E) Survival with identical treatment groups but with treatment delayed until day 10 after tumor inoculation. Mice received (●) rat IgG control, (▪) 250 µg of anti-CD20 mAb (CAT-13) on day 10 and once per week for 3 weeks, and (▲) 200 µg of anti-Ly49C/I F(ab′)2 (5E6) on day 10 and biweekly for 3 weeks, or (♦) the combination of both antibodies. *P = .005.
Anti-Ly49C/I F(ab′)2enhances the antilymphoma activity of anti-CD20 mAb in vivo and is NK-cell–dependent. (A) C57BL/6 mice were inoculated retro-orbitally with 0.5 × 106 EL4-huCD20 lymphoma tumor cells. (B) After tumor inoculation, mice received (●) rat IgG control, (▪) 250 µg of anti-CD20 mAb (CAT-13) on day 3 and once per week for 3 weeks, (▲) 200 µg of anti-Ly49C/I F(ab′)2 (5E6) on day 3 and twice a week for 3 weeks, or (♦) the combination of both antibodies. Mice were then monitored for overall survival. *P = .042. (C) C57BL/6 mice were inoculated retro-orbitally with 0.5 × 106 EL4-huCD20 lymphoma tumor cells. (D) After tumor inoculation, mice received (●) rat IgG control on day 3; (▪) 50 µL of anti-Asialo-GM1 on days −1, 0, 5, 10, 15, 20, and 25 with 250 µg of anti-CD20 mAb and 200 µg anti-Ly49C/I F(ab′)2 on day 3; (▼) 200 µL liposomal clodronate on day −2 followed by 100 µL of liposomal clodronate on days 0, 4, 8, 12, 16, 20, and 24 with 250 µg of anti-CD20 mAb and 200 µg of anti-Ly49C/I F(ab′)2 on day 3; (♦) 500 µg anti-CD8 mAb on days −1, 0, 5, 10, 15, 20, and 25 with 250 µg of anti-CD20 mAb and 200 µg anti-Ly49C/I F(ab′)2 on day 3; or (▲) 250 µg of anti-CD20 mAb on day 3 and 200 µg of anti-Ly49C/I F(ab′)2 on day 3 with 250 µg of anti-CD20 mAb repeated once per week for 3 weeks and 200 µg of anti-Ly49C/I F(ab′)2 repeated biweekly for 3 weeks. Mice were then monitored for overall survival. *P < .001. All in vivo models were piloted with 5 mice per group and repeated with 10 mice per group. Isotype controls included 5% normal mouse serum and 250 µg of 4D11 (Ly49G2) on day 3 and biweekly for 3 weeks in addition to rat IgG with no effect on tumor growth or survival (representative control, rat IgG, shown). (E) Survival with identical treatment groups but with treatment delayed until day 10 after tumor inoculation. Mice received (●) rat IgG control, (▪) 250 µg of anti-CD20 mAb (CAT-13) on day 10 and once per week for 3 weeks, and (▲) 200 µg of anti-Ly49C/I F(ab′)2 (5E6) on day 10 and biweekly for 3 weeks, or (♦) the combination of both antibodies. *P = .005.
Antilymphoma activity of combination therapy requires NK cells
To further investigate the mechanism of action of anti-CD20 mAb and anti-Ly49C/I F(ab′)2 and to confirm the role of NK cells in the therapeutic effect, we next performed a depletion experiment. We found that NK-cell, and not macrophage, CD4, or CD8 T-cell depletion, abrogated the therapeutic efficacy of anti-CD20 mAb and anti-Ly49C/I F(ab′)2 combination therapy (Figure 2C-D).
Blockade of KIR2DL3/HLA-C interaction induces tumor cell killing by NK cells in vitro
To study the therapeutic effect of KIR-targeting antibody in preclinical models, we generated transgenic mice for human KIR2DL3 on a Rag1KO background.9,10 We have previously shown that all NK cells from these Rag1KO-Tg KIR mice express functional KIR2DL3 receptors9 (supplemental Figure 1A on the Blood Web site). Lirilumab binding to these Tg NK cells was dose-dependent (supplemental Figure 1B). To set up in vivo tumor models, we also generated 221 HLA-Cw3 cells, a human B-cell lymphoma overexpressing HLA-Cw3, one of the ligands for KIR2DL3 compared with 221 tumor cells, which express endogenously low levels of MHC-I molecules at their surface (supplemental Figure 1C). Freshly isolated Rag1KO-Tg KIR splenocytes failed to kill 221 cells in vitro (supplemental Figure 1D, left panel), while phospho–isotype control (pIC)–activated splenocytes killed 221 cells (supplemental Figure 1D, middle panel), and this occurred in an NK-cell–dependent manner, as shown by the absence of lysis with NK-cell–depleted splenocytes (supplemental Figure 1D, right panel). HLA-Cw3 expression protected 221 tumor cells from pIC-activated splenocyte killing (supplemental Figure 1D, middle panel). The addition of increasing doses of lirilumab in vitro restored the killing of 221 HLA-Cw3 cells by KIR Tg NK cells in a dose-dependent manner (supplemental Figure 1D, left and middle panels).
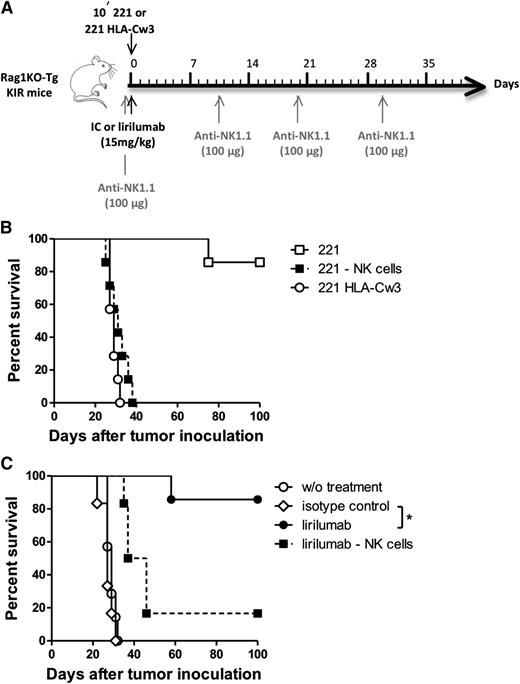
KIR2DL3 engagement on NK cells by tumor MHC-I mediates tumor escape in vivo
Rag1KO-Tg KIR mice lacking T and B cells can be engrafted with various human tumor cell lines, allowing the evaluation in a murine model of anti-KIR antibody that targets NK cells. When Rag1KO-Tg KIR mice were injected intravenously with 221 cells, the majority rejected the tumor and did not show any clinical signs of disease over a 100-day period (Figure 3A-B). The depletion of NK cells in these mice induced the death of mice in a median of 31 days (range, 25 to 38 days), demonstrating that NK cells are involved in 221 tumor growth control in Rag1KO-Tg KIR mice. When 221 HLA-Cw3 cells were injected intravenously into Rag1KO-Tg KIR mice, these cells induced death in a median of 29 days (range, 27 to 32 days). The engagement of KIR2DL3 by HLA-Cw3 is therefore sufficient to inhibit NK cell control of 221 tumor cells in vivo.
Lirilumab therapy improves survival in a prophylactic HLA+tumor model in an NK-cell–dependent manner. (A) Schema of antibody administration. (B) To determine whether HLA+ tumors escape NK-cell control in KIR Tg mice, (□) 221 (n = 7) or (○) 221 HLA-Cw3 (n = 7) tumor cells (107 cells) were injected intravenously into Rag1KO-Tg KIR mice, including (▪) one group injected with 221 tumor cells (107 cells) in which NK cells were depleted with 100 µg of anti-NK1.1 mAb (n = 7). (C) Rag1KO-Tg KIR mice were injected intravenously with 221 HLA-Cw3 tumor cells (107 cells) and subsequently received either (○) no treatment (n = 7), (♢) IC mAb at 15 mg/kg, (●) lirilumab at 15 mg/kg (n = 6), or (▪) lirilumab at 15 mg/kg and 100 µg anti-NK1.1 mAb (n = 6) to deplete NK cells. NK-cell depletion was started on the day prior to tumor challenge and was maintained by injecting 100 µg anti-NK1.1 every 10 days. Mice were then monitored for overall survival. *P < .001. (B) and (C) show several groups of the same experiments. One experiment representative of 3 experiments is shown.
Lirilumab therapy improves survival in a prophylactic HLA+tumor model in an NK-cell–dependent manner. (A) Schema of antibody administration. (B) To determine whether HLA+ tumors escape NK-cell control in KIR Tg mice, (□) 221 (n = 7) or (○) 221 HLA-Cw3 (n = 7) tumor cells (107 cells) were injected intravenously into Rag1KO-Tg KIR mice, including (▪) one group injected with 221 tumor cells (107 cells) in which NK cells were depleted with 100 µg of anti-NK1.1 mAb (n = 7). (C) Rag1KO-Tg KIR mice were injected intravenously with 221 HLA-Cw3 tumor cells (107 cells) and subsequently received either (○) no treatment (n = 7), (♢) IC mAb at 15 mg/kg, (●) lirilumab at 15 mg/kg (n = 6), or (▪) lirilumab at 15 mg/kg and 100 µg anti-NK1.1 mAb (n = 6) to deplete NK cells. NK-cell depletion was started on the day prior to tumor challenge and was maintained by injecting 100 µg anti-NK1.1 every 10 days. Mice were then monitored for overall survival. *P < .001. (B) and (C) show several groups of the same experiments. One experiment representative of 3 experiments is shown.
KIR-HLA interaction blockade induces Tg KIR mouse protection from HLA+ tumor challenge
First, we tested the effect of a single injection of lirilumab given the same day as a tumor challenge with the HLA+ cell line 221 HLA-Cw3. When mice were pretreated with lirilumab (15 mg/kg) a few hours before injection of tumor cells (Figure 3C), 6 of 7 mice survived over a 100-day period (Figure 3C), whereas untreated or IC-treated mice all died in a median of 29 and 27 days, respectively (range, 22 to 32 days). This protection conferred by KIR-MHC-I blockade is at least partly mediated by NK cells, since the depletion of this cell population in lirilumab-treated mice induced the death of 5 of 6 of the mice in a median of 41.5 days (range, 35 to 46 days).
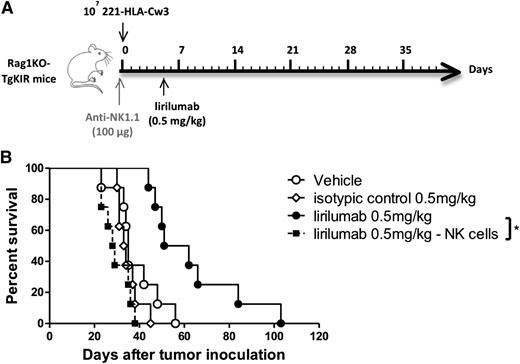
Therapeutic efficacy of anti-KIR administration in vivo
A KIR occupancy study with lirilumab was carried out in Rag1KO-Tg KIR mice to define the dose of lirilumab to be injected into mice according to the required KIR saturation duration (supplemental Figure 2). We then tried to delay mouse treatment with lirilumab 5 days after HLA+ tumor engraftment. Several doses of anti-KIR mAb were tested in single injections (supplemental Figure 3A) and at 0.5 mg/kg, corresponding to 1-day complete KIR saturation on NK cells (supplemental Figure 2); a significant prolongation in survival was observed compared with mice who did not receive lirilumab (supplemental Figure 3B). Here, we showed that in vivo KIR-HLA interaction blockade with a suboptimal dose of 0.5 mg/kg of lirilumab, even 5 days after HLA+ tumor-cell injection, significantly improved the outcome of the disease in KIR Tg mice. The role of NK cells in tumor control was investigated by depleting this population just before tumor cell injection (Figure 4A). When NK cells were depleted, lirilumab treatment did not have any beneficial effect on mouse survival compared with untreated mice (Figure 4B).
Lirilumab therapy improves survival in a therapeutic HLA+tumor model in an NK-cell–dependent manner. (A) Schema of lirilumab administration. (B) To determine therapeutic efficacy of anti-KIR mAb therapy and the role of NK cells, 221 HLA-Cw3 tumor cells (107 cells) were injected intravenously into Rag1KO-Tg KIR mice and, starting 5 days after tumor challenge, groups (n = 8 mice per group) received (○) no treatment, (♢) isotype control at 0.5 mg/kg, (●) lirilumab at 0.5 mg/kg, or (▪) lirilumab at 0.5 mg/kg and 100 µg anti-NK1.1 mAb to deplete NK cells starting on the day prior to tumor inoculation. Mice were then monitored for overall survival. *P = .0002. One experiment representative of 2 experiments is shown.
Lirilumab therapy improves survival in a therapeutic HLA+tumor model in an NK-cell–dependent manner. (A) Schema of lirilumab administration. (B) To determine therapeutic efficacy of anti-KIR mAb therapy and the role of NK cells, 221 HLA-Cw3 tumor cells (107 cells) were injected intravenously into Rag1KO-Tg KIR mice and, starting 5 days after tumor challenge, groups (n = 8 mice per group) received (○) no treatment, (♢) isotype control at 0.5 mg/kg, (●) lirilumab at 0.5 mg/kg, or (▪) lirilumab at 0.5 mg/kg and 100 µg anti-NK1.1 mAb to deplete NK cells starting on the day prior to tumor inoculation. Mice were then monitored for overall survival. *P = .0002. One experiment representative of 2 experiments is shown.
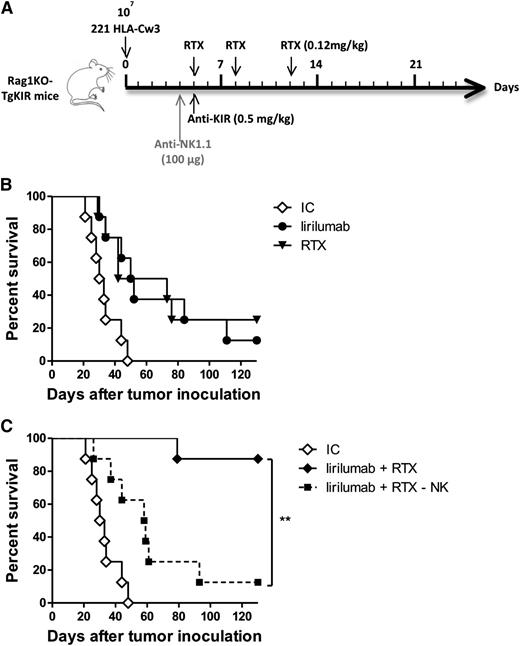
Therapeutic efficacy of anti-KIR and anti-CD20 combination in vivo
Having shown that lirilumab treatment 5 days after tumor challenge could significantly improve mouse survival, we then asked whether this treatment could be combined with rituximab. The 221 HLA-Cw3 cells are of human B-cell origin, and they express CD20 at their cell surface (supplemental Figure 1C). We assessed the efficacy of suboptimal doses of rituximab or lirilumab alone (Figure 5A). Median survival of mice challenged with 221 HLA-Cw3 cells and treated with both ICs was 31.5 days (range, 21 to 48 days) and increased to 57.5 days (range, 29 to 76 days) with rituximab treatment and to 51 days with anti-KIR treatment (range, 30 to 111 days) (Figure 5B). When both treatments were combined at suboptimal doses (Figure 5A), almost all mice survived to tumor challenge for at least 130 days (Figure 5C). NK cell depletion the day before the start of the treatments completely abrogated the benefit of treatment combination, with mice dying in a median of 58.5 days (range, 26 to 93 days), showing that NK cells are necessary for the combinational effect of both treatments (Figure 5C).
Lirilumab therapy enhances the antilymphoma activity of rituximab in vivo and is NK-cell–dependent. (A) Schema of lirilumab and rituximab administration. (B) To determine the therapeutic efficacy of drug combination vs monotherapy, 221 HLA-Cw3 tumor cells (107 cells) were injected intravenously into Rag1KO-Tg KIR mice. Starting 5 days after tumor challenge, groups (n = 8 mice per group) received (♢) IC, (●) lirilumab intravenously at 0.5 mg/kg on day 5, or (▼) rituximab (RTX) intraperitoneally at 0.12 mg/kg on days 5, 8, and 12. Mice were then monitored for overall survival. (C) To determine the role of NK cells, 221 HLA-Cw3 tumor cells (107 cells) were injected intravenously into Rag1KO-Tg KIR mice and, starting 5 days after tumor challenge, groups (n = 8 mice per group) received (♢) IC, (♦) lirilumab at 0.5 mg/kg on day 5 and RTX at 0.12 mg/kg on days 5, 8, and 12, or (▪) lirilumab at 0.5 mg/kg on day 5 and RTX at 0.12 mg/kg on days 5, 8, and 12 and 100 µg of anti-NK1.1 mAb on day 4 to deplete NK cells. Mice were then monitored for overall survival. *P < .001. (B) and (C) show several groups of the same experiments. One experiment representative of 2 experiments is shown.
Lirilumab therapy enhances the antilymphoma activity of rituximab in vivo and is NK-cell–dependent. (A) Schema of lirilumab and rituximab administration. (B) To determine the therapeutic efficacy of drug combination vs monotherapy, 221 HLA-Cw3 tumor cells (107 cells) were injected intravenously into Rag1KO-Tg KIR mice. Starting 5 days after tumor challenge, groups (n = 8 mice per group) received (♢) IC, (●) lirilumab intravenously at 0.5 mg/kg on day 5, or (▼) rituximab (RTX) intraperitoneally at 0.12 mg/kg on days 5, 8, and 12. Mice were then monitored for overall survival. (C) To determine the role of NK cells, 221 HLA-Cw3 tumor cells (107 cells) were injected intravenously into Rag1KO-Tg KIR mice and, starting 5 days after tumor challenge, groups (n = 8 mice per group) received (♢) IC, (♦) lirilumab at 0.5 mg/kg on day 5 and RTX at 0.12 mg/kg on days 5, 8, and 12, or (▪) lirilumab at 0.5 mg/kg on day 5 and RTX at 0.12 mg/kg on days 5, 8, and 12 and 100 µg of anti-NK1.1 mAb on day 4 to deplete NK cells. Mice were then monitored for overall survival. *P < .001. (B) and (C) show several groups of the same experiments. One experiment representative of 2 experiments is shown.
Discussion
Since the approval of rituximab by the US Food and Drug Administration in 1997, mAbs have become standard of care for the treatment of both solid tumors and hematologic malignancies.24 Despite favorable toxicity profiles, target specificity, and up-front response rates, in patients with advanced disease or those who have previously been heavily treated, mAbs have limited clinical activity with response rates of 10% or less.25 Therefore, a major translational research effort is the identification of new combination approaches to enhance the efficacy of mAbs.
The ability of combination approaches to enhance mAb activity is largely determined by the capacity to augment ADCC and the degree to which a given mAb’s mechanism of action requires ADCC. Clinical series among patients with lymphoma treated with rituximab,17,18 among patients with human epidermal growth factor receptor 2–expressing breast cancer treated with trastuzumab,26 or patients with colorectal cancer treated with cetuximab27,28 showed a correlation between clinical benefit and FcγRIIIa genotype—patients who had higher affinity polymorphisms demonstrated superior clinical outcomes. In contrast, the anti–epidermal growth factor receptor mAb panitumumab does not induce ADCC because of a different isotype that does not bind to the FcγRIIIa. Therefore, when considering enhancement of ADCC, such approaches are limited to combinations with mAbs that trigger the Fc receptor.
Understanding mechanisms of mAb resistance may offer insight into strategies to enhance ADCC. Interestingly, in vitro, HLA density and not CD20 expression has been shown to correlate with rituximab efficacy and NK-cell capacity for ADCC.29 Increased expression of HLA class I molecules results in a masked tumor cell appearing as “self” and in inhibition of NK-cell cytotoxicity through KIR interactions.29 More recently, the therapeutic activity of an ADCC-dependent mAb targeting the disialoganglioside GD2 in neuroblastoma was shown to be mediated by KIR-mismatched NK cells.30 In this study, ADCC from KIR-positive NK cells was shown to be inhibited by HLA cognate interaction, but this inhibition was reversible by the addition of anti-HLA Abs in vitro,30 supporting the rationale of blocking KIR to enhance the ADCC effect of therapeutic antibodies.31 Furthermore, in human patients, lirilumab targets several KIRs—KIR2DL1, -L2, -L3, -S1, and -S2—expressed on half of the total NK-cell population. The inhibitory KIRs targeted by lirilumab collectively recognize virtually all HLA-C alleles, and the blockade of all three KIR2DLs allows treating all patients without prior HLA or KIR typing.9,12,32
Therefore, we investigated the efficacy of a treatment regimen that included lirilumab-mediated KIR blockade and the therapeutic mAb rituximab in the hope that such a combination would augment ADCC and improve response rates and prevent resistance and tumor escape.
We developed two CD20+ lymphoma models to evaluate the combination of anti-KIR and anti-CD20 mAb therapy. By transfecting a murine lymphoma (EL-4) with human CD20, we could assess in vitro and in vivo the efficacy of the combination of anti-CD20 mAb and blockade of the murine homolog of human KIRs (the Ly49 family) by using F(ab′)2 fragments of the anti-Ly49C/I mAb22 in an immune competent system. To study the therapeutic effect of blocking KIR2Ds with lirilumab, we used KIR2DL3 Tg mice on a Rag1KO background.9,10 To investigate combination therapy with anti-CD20 mAb, we generated 221 HLA-Cw3 cells, a human B-cell lymphoma transfected with HLA-Cw3 (one of the ligands for KIR2DL3). The 221 HLA-Cw3 cells express high levels of HLA molecules at their surface as well as CD20 and therefore are targeted by both anti-KIR and anti-CD20 mAbs.
Our findings in vitro confirm prior studies on human cells showing enhancement of anti-CD20 mAb-mediated lysis of CD20-expressing lymphoma cell lines by KIR blockade.33,34 The results reported here illustrate that, when combined in vivo, treatment with rituximab plus lirilumab or anti-Ly49C/I mAbs augments NK cell activity. Depletion of NK cells abrogated the benefit of combination therapy. It was also previously reported that KIR inhibition enhanced cytotoxicity in an autologous system by using effector NK cells and Epstein-Barr virus–transformed B cells as target cells from the same donor.9 Combined with our findings, this supports that KIR-Ly49 blockade enhances both murine and human NK-cell ADCC.33
Our approach supported here is one of several strategies to improve the innate immune response following Fc receptor activation by an mAb.35 Focusing on NK cells as a major effector cell responsible for ADCC, initial investigation tested the hypothesis that increasing NK-cell numbers ex vivo could enhance the antitumor activity of an mAb. Adoptive transfer of lymphokine-activated killer cells in a cohort of patients with rituximab-refractory lymphoma improved NK-cell counts in peripheral blood and ADCC and even induced clinical responses in some patients.36 In contrast to our approach, adoptive transfer of NK cells is labor- and cost-intensive. It has possible biologic limitations resulting from the removal, isolation, and transfer of NK cells which can lead to NK exhaustion as a result of downregulation of transcription factors such as eomesodermin and T-cell-specific T-box transcription factor.37
Cytokine-based approaches to enhance NK-cell number and function in vivo without adoptive transfer have been investigated clinically, although few combination trials with mAbs have demonstrated superiority to monotherapy.38 Likely a result of the systemic, generalized immune stimulation, most cytokine therapies are accompanied by systemic toxicity. Another possibility for enhancing rituximab-induced killing by NK cells is the combination with lenalidomide, an immunomodulatory drug approved for the treatment of multiple myeloma and myelodysplastic syndrome, which enhances ADCC against CD20-expressing B-cell chronic lymphocytic leukemia primary cells through increased granzyme B and Fas ligand expression.39
As an alternative to enhancing ADCC, lenalidomide was also combined with anti-KIR mAb strategy, and it potentiated NK-cell cytotoxicity toward autologous myeloma cells in vitro.10 This combination is currently being investigated in a phase 1 clinical trial in multiple myeloma patients (NCT01217203).40
In contrast to the anti-KIR combination mAb strategy, which removes an inhibitory checkpoint, we have recently reported use of an agonistic NK-cell–targeted mAb to augment ADCC. Following FcR triggering during ADCC, expression of the activation marker CD137 is increased.41 Agonistic antibodies targeting CD137 in preclinical models, both in vitro and in vivo, augment NK-cell function, including degranulation, secretion of IFN-γ, and antitumor cytotoxicity.42-44 The combination of anti-CD137 antibody approach with rituximab is currently being evaluated in a phase 1 trial in patients with lymphoma (NCT01307267).42,43,45,46
Multiple efforts to enhance mAb efficacy, including adoptive NK-cell therapy, systemic cytokine, or immunomodulatory drug administration, and agonistic antibody combinations are currently in active clinical investigation. A first-in-class therapy capable of augmenting ADCC has yet to be successful in late-stage clinical trials. We present here preclinical evidence supporting another novel approach to enhancing mAb antitumor efficacy. Our findings provide a rationale for the combination of an anti-KIR mAb to “remove the brakes” from NK cells and further enhance the efficacy of rituximab among other mAbs by augmentation of ADCC. A clinical trial investigating this strategy is needed.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Yannis Morel for initiating the collaboration between both teams and for helpful discussions, Claude Bagnis (Etablissement Français Du Sang Marseille) for providing lentiviral particles used to generate 221 cell transfectants, and Benjamin Rossi (Innate Pharma) for plasmid constructs.
This work was supported by the National Institutes of Health (CA34233 and CA33399). H.E.K. is supported by the Leukemia and Lymphoma Society, American Society of Hematology, American Society of Clinical Oncology, and Damon Runyon Foundation. Laboratory support (E.V.) is provided by the European Research Council (THINK Advanced Grant) and by institutional grants from Institut National de la Santé et de la Recherche Médicale, Centre national de la recherche scientifique, and Aix Marseille University (Centre d’Immunologie de Marseille-Luminy).
Authorship
Contribution: H.E.K., A.T., and C.S. designed and performed experiments, analyzed data, and wrote the paper; F.C., N.F., A.R., D.C., E.W., A.M., and I.S.-B. performed experiments; C.B., S.U., E.V., and F.R. designed experiments and reviewed data; and M.B., P.A.. and R.L. designed experiments, reviewed data, and wrote the paper.
Conflict-of-interest disclosure: A.T., C.S., F.C., N.F., C.B., F.R., P.A., and M.B. are employees of Innate Pharma. E.V. and F.R. are co-founders of Innate Pharma. The remaining authors declare no competing financial interests.
Correspondence: Holbrook E. Kohrt, Division of Oncology, 269 Campus Dr, CCSR 1145, Stanford University Medical Center, Stanford, CA 94305-5151; e-mail: kohrt@stanford.edu; and Pascale André, Innate Pharma, 117 Avenue de Luminy, BP-30191, 13276 Marseille Cedex 09, France; e-mail: pascale.andre@innate-pharma.fr.
References
Author notes
H.E.K., A.T., R.L., M.B., and P.A. contributed equally to this study.