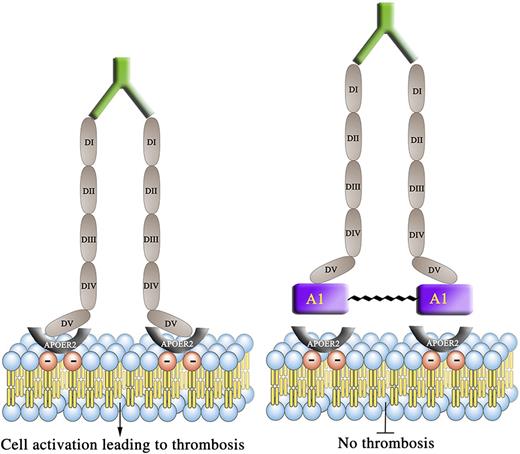
Dimerization of β2GPI by anti-β2GPI autoantibodies from humans and mice that spontaneously develop APS potentiate thrombus formation in vivo which is attenuated by the A1-A1 inhibitor. A1-A1, inhibitor of dimeric β2GPI immune complexes; DI-DV, domain 1-5 of β2GPI. (Symbols) Green prong, anti-β2GPI autoantibodies; red circle with minus, negative-charged phospholipid; gray half circle (U shape), ApoER2.
Dimerization of β2GPI by anti-β2GPI autoantibodies from humans and mice that spontaneously develop APS potentiate thrombus formation in vivo which is attenuated by the A1-A1 inhibitor. A1-A1, inhibitor of dimeric β2GPI immune complexes; DI-DV, domain 1-5 of β2GPI. (Symbols) Green prong, anti-β2GPI autoantibodies; red circle with minus, negative-charged phospholipid; gray half circle (U shape), ApoER2.
APS is an important cause of acquired thrombophilia in the community, characterized by predisposition to both venous and arterial thrombosis, as well as obstetric complications. The laboratory diagnostic criteria for APS require the demonstration of persistently elevated levels of so-called antiphospholipid antibodies (aPL Abs) detected either by the anticardiolipin (aCL) or anti-β2GPI enzyme-linked immunosorbent assays (ELISAs) or lupus anticoagulant assays (LACs).2 The term aPL Abs is a misnomer, as the major autoantigen to which APS patient autoantibodies (Abs) bind is β2GPI, a plasma protein that binds to negatively charged phospholipids such as cardiolipin.3 Anti-β2GPI Abs bind domain I of the β2GPI molecule4 (see figure).
Patient-derived anti-β2GPI Abs mediate direct thrombogenic effects via multiple mechanisms, which have been delineated using both in vitro and in vivo experiments (extensively reviewed elsewhere).5 An important mechanism is the ability of anti-β2GPI Abs to dimerize β2GPI molecules on a number of cell-surface receptors leading to activation of prothrombotic downstream pathways in platelets, endothelial cells, and monocytes. One such receptor on platelets is ApoER2 (see figure). The in vivo importance of this receptor has been delineated using ApoER2 knockout mice, whereby the ability of passively transferred Abs from APS patients to potentiate thrombosis was abrogated in the knockout mice compared with the wild type.6
Kolyada and colleagues have used, in an innovative way, insights gleaned from previous work which has shown that β2GPI via its fifth domain binds the A1 portion of ApoER2.7 They have synthesized a dimer, composed of 2 A1 molecules joined by a flexible linker, and have demonstrated its ability to inhibit anti-β2GPI Ab/dimerized β2GPI complexes from binding negatively charged phospholipids and ApoER2 in vitro, in a manner that is more potent than using A1 in the monomeric form.8 A previous study by the research group of the late Silvia Pierangeli demonstrated that the A1 monomer is able to effectively inhibit thrombus potentiation induced by the passive infusion of Abs from APS patients into a nonautoimmune murine thrombosis model.6 One of the key questions that remained for Kolyada and colleagues, in order for them to extend their in vitro work,8 was whether the A1 dimer they have developed is effective in ameliorating anti-β2GPI Ab-mediated thrombus potentiation in vivo.
In this study, the research group of Kolyada, Porter, and Beglova have addressed this question using 2 distinct murine APS in vivo thrombosis models.1 They studied the effects of A1-A1 and control peptide on laser-induced thrombus size in the autoimmune strain, NZW × BXSB yaa F1 male mice. This murine strain is significant because it is the only known strain that spontaneously develops a syndrome that is analogous to human APS on a background of systemic lupus erythematosus.9 The male mice spontaneously develop aPL Abs, including anti-β2GPI Abs, with epitope specificity identical to anti-β2GPI Abs affinity purified from APS patients.4,10 Kolyada et al determined that significant levels of anti-β2GPI Abs spontaneously develop at ∼8 weeks of age in this strain of male mice, rising further at 10 weeks of age, then staying at a plateau between 10 and 16 weeks.1 Thrombus-inducing laser injuries to the cremasteric arteriolar vessels were administered in a systematic manner to mice aged between 13 and 14 weeks, allowing comparison of median thrombus size in mice before and after being given either A1-A1 or placebo. The A1 dimer significantly inhibited thrombus formation. Of note, when a laser injury was administered to mice aged 6 weeks old, that is, prior to the development of anti-β2GPI Abs, there was no difference in median thrombus size between the mice administered A1-A1 and those given placebo, emphasizing that the A1 dimer specifically inhibits anti-β2GPI Ab-mediated thrombosis.1
The other murine APS model used is characterized by the passive infusion of affinity purified anti-β2GPI immunoglobulin G (IgG) Abs purified from the serum of a thrombotic APS patient (positive on the aCL and anti-β2GPI ELISAs and LACs) into a nonautoimmune mouse strain (BALB/C), followed by a set of laser injuries before and after mice are treated with either A1-A1 or control peptide. The A1 dimer significantly inhibited patient anti-β2GPI IgG Ab-mediated murine thrombus potentiation.1
These findings provide important proof of concept of the potential therapeutic utility of A1-A1 being used to prevent anti-β2GPI–mediated thrombosis in individuals who are at risk of suffering an APS-related thrombotic event. However, many issues will need to be addressed before realizing the potential of this therapy. In the study, the drug was administered intravenously, and for it to realistically be used as a long-term strategy in APS patients, an oral preparation for ease of administration would be an important development. Patient selection will also be relevant should A1-A1 be used in the primary prevention setting for patients at high risk for APS thrombosis or as a secondary prevention treatment once thrombosis has occurred? In the secondary prevention setting at what point will it be safe to switch from a standard anticoagulant to A1-A1? Does the A1 dimer have any potential therapeutic utility for preventing obstetric APS complications such as recurrent first-trimester miscarriages, second-trimester fetal death, or APS-related severe preeclampsia? Despite the significant number of uncertainties and hurdles ahead for the development of A1-A1 as a therapy in human APS, this study represents an important step in its development as a candidate therapy for targeting a disease-specific mechanism of thrombus formation in APS.
Conflict-of-interest disclosure: The authors declare no competing financial interests.