Abstract
Background
Multiple myeloma (MM) remains an incurable plasma cell neoplasm with >20,000 new cases diagnosed annually in the United States (US). The presentation of MM is diverse and the management is guided by disease- and patient- related factors. Real world evidence regarding disease presentation is sparse for newly diagnosed MM (NDMM) patients. The goal of this study was to describe the baseline demographic and clinical characteristics of NDMM patients by linking multiple large claims databases in the US.
Methods
A retrospective cohort study was conducted by linking the records between 01/01/2006-12/31/2013 from three longitudinal IMS databases (Medical Claims, Pharmacy Prescriptions, and Hospital Charge Master), to reflect a complete treatment continuum for patients in all ages and by all payer types across healthcare settings. Included patients met the following criteria: ≥2 claims with a diagnosis of MM (ICD-9-CM 203.0x) at least 30 days apart between 01/01/2007-12/31/2012 (first MM diagnosis date = index date); provider stability for at least 6 months before and 3 months after index date; aged 18+ as of index date. NDMM patients were identified as those with no MM diagnosis in the 6 months pre-index.
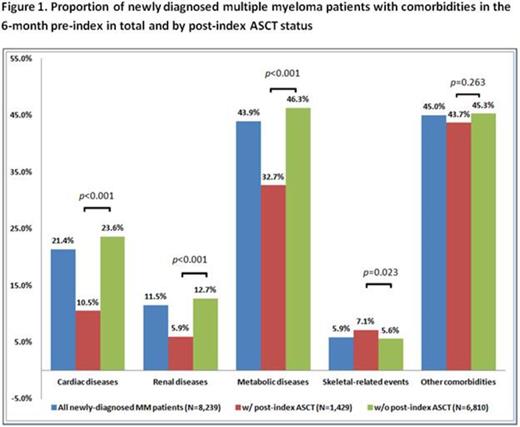
Patient baseline characteristics were assessed using data at index for age, gender, geographic region and payer type; 6-month pre-index plus index day data for Charlson Comorbidity Index (CCI); 6-month pre-index data for 32 comorbidities (e.g., cardiac arrhythmia, cerebrovascular disease, chronic kidney disease, diabetes, hypertension, among others); and 5 comorbidity categories (cardiovascular, renal, metabolic, skeletal-related events, and other). Autologous stem cell transplant (ASCT) status was also assessed based on the available follow-up data after initial diagnosis. Patient baseline characteristics were compared between the patients with versus without ASCT after MM diagnosis. Chi-square tests for categorical variables and t-tests for continuous variables (alpha=0.05) were conducted.
Results
The study cohort of 8,239 NDMM patients had a mean (SD) age of 66.2 (11.3) years at diagnosis, with 56.7% aged 65+; 51.8% were female; and the majority were with commercial (43.3%) or Medicare (42.8%) as payer. Patients with post-index ASCT (n=1,429; 17.3%) were distinctly different from those without (n=6,810; 82.7%): they were younger with a mean (SD) age of 58.1 (8.7) vs. 67.9 (11.1) years, fewer aged 65+, 24.1% vs. 63.5%; fewer female, 47.6% vs. 52.6% (all p<0.001); and the majority (67.5%) of patients who later had ASCT were covered by commercial plans, compared to Medicare as the biggest payer (48.2%) for those who did not have post-index ASCT.
NDMM patients had an overall mean (SD) CCI score of 3.1 (1.6). Patients who later received ASCT were healthier than those who did not, with mean (SD) CCI scores of 2.7 (1.4) vs. 3.2 (1.6) (p<0.001). Close to half (47.9%) of all NDMM patients had >1 type of comorbidities at baseline. Figure 1 depicts the baseline comorbidity categories among all NDMM patients as well as the two subsets (with versus without post-index ASCT). Comorbidities were prevalent even before MM diagnosis: 43.9% of patients presented with metabolic comorbidities, 21.4% with cardiovascular diseases, 11.5% with renal conditions, 5.9% with skeletal-related events, and 45.0% with other comorbidities. The patient subset with post-index ASCT had lower comorbidity occurrences compared to those without: 10.5% vs. 23.6% in cardiovascular diseases, 5.9% vs. 12.7% in renal conditions, 32.7% vs. 46.3% in metabolic diseases (all p<0.001), consistent with literature showing that ASCT candidates tend to be younger and have less severe comorbidities.
Conclusions
This study provided baseline demographic and comorbidity profiles of NDMM patients and showed that the NDMM patient population presented with various comorbidities prior to the first MM diagnosis, suggesting the needs for efficacious, tolerable and safe treatment options for a heterogeneous patient population with complex disease profiles. As expected, patients who had ASCT after initial diagnosis were younger and healthier than those who did not have ASCT. The study findings portray a clearer picture of NDMM patients in the US, and provide clinicians with valuable real world evidence to identify appropriate treatment strategies for these patients.
Chen:Onyx Pharmaceuticals: Research Funding. De:Onyx Pharmaceuticals: Research Funding. Cong:Onyz Pharmaceuticals: Employment. Aggarwal:Onyx Pharmaceuticals: Employment. Wade:Onyx Pharmaceuticals: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal