Abstract
Stroke and its neurocognitive sequelae are devastating complications of sickle cell disease (SCD). Cerebral blood flow (CBF), a measure of tissue specific blood flow in the brain, is a key part of cerebral metabolism, and can provide insight into the pathophysiology of the neurologic complications of SCD. Previous work suggests that CBF is elevated in SCD patients compared to healthy controls (HC). Elevated CBF likely represents a compensatory mechanism to maintain cerebral oxygen delivery and metabolism in the setting of decreased arterial oxygen content secondary to chronic anemia. Previous studies are limited by small sample size and variations in imaging technique, making meta-analysis an alluring method for obtaining large numbers of participants to determine and compare population norms. Therefore, we performed a systematic meta-analysis to establish normal CBF values as measured by arterial spin labeled perfusion MR imaging (ASL) in pediatric HC and SCD populations, hypothesizing that CBF would be elevated in children with SCD when compared to a HC cohort.
A systematic literature search was performed in 02/2014 for the HC cohort, and 06/2014 for the SCD cohort in Medline, Embase, and CINAHL. Whole brain cerebral blood flow (WB-CBF) measurements obtained by ASL in participants from 1 - 18 years (yr) were necessary for inclusion in both cohorts, and a diagnosis of hemoglobin SS or hemoglobin S-Beta thalassemia null for inclusion in the SCD cohort. ASL is the preferred imaging modality for CBF in pediatrics because ASL non-invasively measures CBF without the use of an exogenous contrast agent or ionizing radiation exposure. Data was excluded from the HC cohort if a medical disorder known to affect CBF was reported. Analysis included determination of mean WB-CBF values weighted by the inverse variance with 95% confidence intervals (CI) stratified by mean age, which was categorized as 1-9 yr and 9-18 yr secondary to known CBF changes throughout development. Statistical heterogeneity, or between-study variability, was assessed with Cochrane's Χ2 and I2. An I2 value greater than 30% was used as the threshold for analysis with a random-effects model. A funnel plot of the effect estimates versus the sample size for each individual study was used to assess for publication bias. Metaregression was used to determine the contribution of covariates to between-study heterogeneity in measurements of WB-CBF. All analyses were performed with STATA 13.1 (College Station, Texas) using the METAN software package.
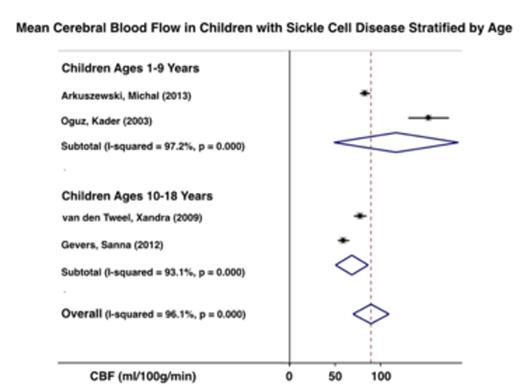
The literature search produced 155 articles for HC patients, and 12 articles for SCD patients; 8 publications met the inclusion and exclusion criteria for the HC cohort (89 children) and 4 publications for SCD cohort (92 children). Between the ages of 1 – 9 yr, mean WB-CBF in HC children was 67.6 ml/100 g/min (95% CI 37.9, 97.2), and mean WB-CBF in children with SCD was 117.0 ml/100 g/min (95%CI 48.7, 185.4). Between the ages of 10 – 18 yr, mean WB-CBF in HC children was 60.8 ml/100 g/min (95% CI 37.7, 83.9), and mean WB-CBF in children with SCD was 68.4 ml/100 g/min (95% CI 50.5, 86.3) (figures 1 and 2). The difference between the two cohorts is not statistically significant because of overlapping CI. The CochraneÕs X2 was significant with a p < 0.001 in all 4 analysis, with the I2 for each analysis ranging from 93.1% - 98.9%, indicating significant between-study heterogeneity. Mean age, ASL labeling technique, MRI vendor, and magnet strength, were not significant predictors of between-study heterogeneity within the HC cohort after controlling for multiple comparisons with the Bonferroni correction. Metaregression analysis of the SCD cohort could not be performed secondary to insufficient number of studies. Visual inspection of funnel plots did not provide evidence of publication bias.
Mean WB-CBF as determined by meta-analysis in younger SCD patients is higher than mean WB-CBF in HC children, with little difference seen in older children. These findings suggest that younger children with SCD require increased compensation via elevated CBF to maintain cerebral oxygen metabolism when compared to older children. The significant between-study heterogeneity and wide CI illustrate a need to standardize the ASL technique for CBF measurement within pediatric HC and SCD populations, and the importance of including an age-matched control population when measuring CBF in SCD children.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal