Abstract
Accurate prognostication is essential for patients with myelodysplastic syndromes (MDS) to facilitate optimal patient management. Several systems for predicting the outcome of patients with MDS are commonly used in clinics, including the International Prognostic Scoring System (IPSS), revised IPSS, and a low risk MDS model developed by The University of Texas MD Anderson Cancer Center (MDA). We designed this study to evaluate and compare these three models in lower risk MDS patients in order to accurately identify patients with a poor prognosis who may need early therapeutic intervention.
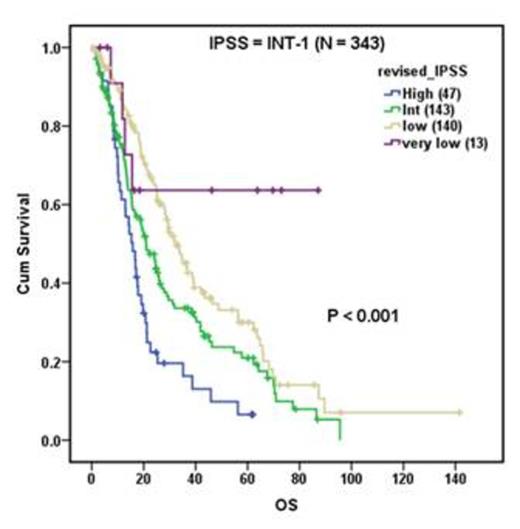
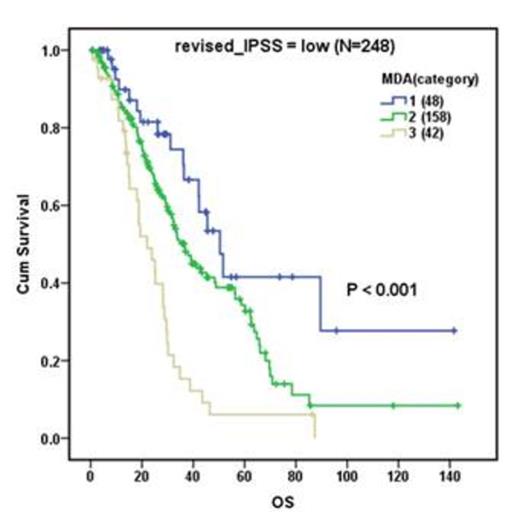
A total of 733 adult patients, median age 69 years (range, 24-91), who were diagnosed as lower risk MDS (IPSS low or intermediate-1) with complete cytogenetic evaluations at MDA were included in this study. Both IPSS and revised IPSS systems stratified the study cohort into groups with significantly different overall survival (OS) (P<0.001 in both). The MDA model further stratified patients into significantly different OS groups (P<0.001), and further stratified the revised IPSS low group (N=248, P<0.001) by OS, but not the very low or intermediate (INT) groups.
Because both IPSS models are heavily weighted toward cytogenetic features, but over half of MDS patients present with normal (diploid) cytogenetics, we compared the effectiveness of these models in risk stratification among diploid MDS patients. Without the effects of cytogenetics, all 3 models still stratified OS significantly (P<0.001 for all). Revised IPSS further stratified IPSS low (N=171, P<0.001) and INT-1 (N=184, P=0.005) into significant different OS groups. The MDA model further stratified IPSS low (P=0.041) and INT-1 (p<0.001) into significant different OS groups. Multivariate analyses showed that age, bone marrow blast count, and hemoglobin and platelet levels were independent factors for survival in all MDS patients and in diploid MDS patients, whereas absolute neutrophil count was not significant for either group.
Molecular markers hold promise for further risk stratification in diploid MDS patients. We assessed the prognostic significance of common gene mutations, such as NPM1, FLT3, DNMT3A, NRAS and KIT. We also identified a signature of plasma microRNAs of which expression levels can predict survival of diploid MDS patients more accurately than all three models.
In summary, the revised IPSS system has improved the stratification of patients in the IPSS low and INT-1 categories. The MDA model improves the OS stratification in IPSS low and INT-1 groups, as well as the revised IPSS low group. All three systems effectively predict survivals in diploid MDS patients. Development of novel molecular markers will enable further risk stratification of MDS patients, especially in the diploid MDS group.
Kantarjian:ARIAD, Pfizer, Amgen: Research Funding. Cooper:InCellerate: Equity Ownership; Sangamo: Patents & Royalties; Targazyme: Consultancy; GE Healthcare: Consultancy; Ferring Pharmaceuticals: Consultancy; Fate Therapeutics: Consultancy; Janssen Pharma: Consultancy; BMS: Consultancy; Miltenyi: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal