Abstract
Introduction: MDS are a diverse group of haematological disorders affecting bone marrow function and necessitating frequent blood transfusions. A number of studies, from retrospective cohort and registry analyses to randomized controlled trials (RCTs), have shown transfusion status to impact OS in MDS. While transfusion status is considered a prognostic indicator in MDS, no systematic review has been conducted to consolidate and analyze all available evidence to date. This systematic review and meta-analysis is the first to assess the association between TI and OS, and also considers patient risk and acquisition of TI post treatment.
Methods: Comprehensive electronic searches were conducted in five key bibliographic databases. Relevant conference proceedings were searched electronically, experts were contacted, grey literature (national and international guidelines, unpublished and unindexed studies) was searched online, and the reference lists of relevant reviews and guidelines were checked. The protocol was published a priori on PROSPERO (ID CRD42014007264).
Studies which recruited adults aged ≥ 18 years with confirmed MDS, and reported OS for TI versus transfusion-dependent (TD) pts were included. Any expression of OS and any definition of transfusion status (x transfusions per unit time) were acceptable. RCTs, cohort studies, consecutive case series ≥ 10 cases, before-after studies and case-control studies were eligible for inclusion. Where a hazard ratio (HR) was expressed for TD vs. TI, the ratio was converted by dividing 1 by the reported HR to obtain HR for TI vs. TD.
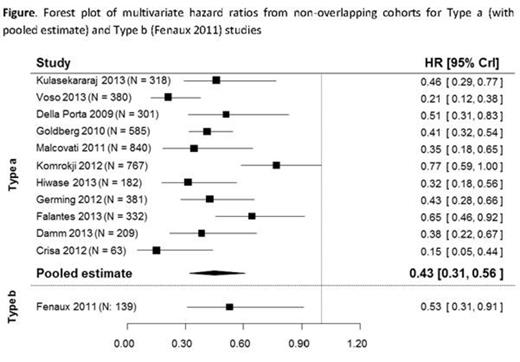
A narrative synthesis and a random effects meta-analysis were conducted. The meta-analysis synthesised the multivariate HR for OS of TI compared with TD pts from non-overlapping cohorts. A random effects meta-regression assessed whether the effect of being TI on OS depends on the risk group (according to IPSS or WHO criteria) of the included pts.
Results: Searches identified 1821 titles of which 89 were included, representing 60 separate analyses. Study quality (by the Quality in Prognosis Studies [QUIPS] criteria) was moderate overall, with some limitations in reporting of attrition, correction of confounders, and patient spectrum. Three types of studies were identified: a) recruited TD and TI pts and compared OS between groups (n = 45); b) recruited TD only, and compared those who became TI to those who remained TD after treatment (n = 8); c) recruited TD only, compared those with high transfusion burden to those with low (n = 7).
Amongst type a studies (n = 45), TI was consistently associated with an OS benefit whether results were expressed as HRs or as other metrics such as mean survival. In a meta-analysis of all eligible type a studies (n = 11) a 57% decrease in the risk of death compared with TD pts (HR 0.43; 95% credible interval (CrI) 0.31 to 0.56) was estimated. When considering the impact of the risk category of pts through meta-regression (lower-risk and all-risk cohorts only; no higher-risk cohorts were eligible for inclusion), the coefficient of the interaction term was estimated to be HR 1.33 (95% CrI 0.6 to 2.98), which suggested that the magnitude of the benefit for pts being TI on OS was higher for all-risk groups. However, this effect was inconclusive.
A meta-analysis of type b studies was not possible as study cohorts overlapped. The multivariate HR in the 3 type b studies which reported this ranged from 0.53 to 0.36, indicating a mortality reduction between 47% and 64% associated with acquisition of TI. Studies reporting other metrics also reported TI pts fared better.
A meta-analysis of type c studies was neither planned nor conducted. All studies reported that pts with fewer transfusions per unit time demonstrated better OS than those with more, regardless of the high/low transfusion burden cut point used.
Conclusion: A number of studies have previously suggested that MDS pts who are TI have better survival relative to those who are TD, but no meta-analysis has been conducted to date. Our findings revealed a consistent, substantial reduction in mortality among TI pts when compared with TD pts confirming the positive TI-OS association. A meta-regression analysis indicated that the impact of TI was higher in all-risk cohorts versus lower-risk cohorts, but this effect was not conclusive. A similar association was seen for those who acquired TI through treatment (Figure 1).
Harnan:Celgene Ltd: Research Funding. Ren:Celgene: Research Funding. Gomersall:Celgene Corporation: Research Funding. Everson-Hock:Celgene Ltd: Research Funding. Dhanasiri:Celgene Corp: Employment, Equity Ownership. Kulasekararaj:Celgene: Honoraria, Speakers Bureau; Alexion: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal