Abstract
Background: Although HMA (azacitidine [aza] or decitabine [dac]) are standard of care therapies for HR-MDS pts, responses may not be seen for 4-6 months and occur in <50% of treated pts. Moreover, curative hematopoietic cell transplantation (HCT), which is recommended as up-front therapy for HR-MDS, is used in <5% of pts. The ability to identify pts with a low likelihood of benefiting from HMA who instead should receive immediate HCT or experimental treatment approaches is a clinical and research priority. Established MDS prognostic systems include the International Prognostic Scoring System (IPSS) and the revised IPSS (IPSS-R) [derived from untreated pt cohorts] and the MD Anderson Prognostic Scoring System (MDAPSS) [derived from treated and untreated pt cohort]. A French Prognostic Scoring System (FPSS) was developed to predict survival among aza-treated HR-MDS pts. We compared the relative prognostic discriminatory power of these models in a large cohort of HMA-treated pts with HR-MDS.
Methods: The combined MDS database obtained from six institutions in the MDS Clinical Research Consortium (Moffitt Cancer Center, Cleveland Clinic, MD Anderson Cancer Center, Dana Farber Cancer Institute, Weill Medical College of Cornell University, and the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins) was used to identify patients with HR-MDS (IPSS intermediate-2 [INT-2] and high) who received HMA therapy (aza or dac). Responses were defined per International Working Group 2006 criteria. Overall response rate (ORR) was defined as the sum of rates of complete response (CR), partial response (PR), hematologic improvement (HI), and marrow CR. Pts with stable disease (SD) and progressive disease (PD) were considered non-responders. Logistic regression models were fitted and tested for association of response with prognostic risk categories using chi-square deviance tests. Overall survival (OS) was calculated from the time of diagnosis to time of death or last follow-up. Kaplan-Meier (KM) curves were generated for OS and the log-rank test was used to compare median OS. Akaike information criteria (AIC) were used to assess the relative goodness of fit of the models.
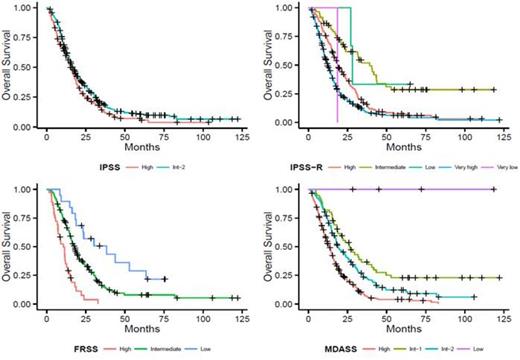
Results: We identified 595 pts with HR-MDS (70.3% with INT-2 and 29.7% with high IPSS) who received HMA as upfront therapy (83% aza, 17% dac). Median follow-up from diagnosis was 13.1 months (M), 95% confidence interval (CI): 11.5-15.1 M. 66% of pts were male, 88% white, 85% were >60 years, and 18% had therapy-related MDS. Median number of HMA cycles was 5.7 (range, 0.7-51) with 75% of pts receiving ≥3 cycles of therapy. Median time from diagnosis to start of HMA therapy was 1.5 M. ORR was 42.1% (CR 25.8%, PR 6.7%, HI-E 3.3%, HI-P 2.3%, HI-N 4.0%) while 57.2% were non-responders (SD 28.6% and PD 28.6%) and 0.7 were un-evaluable. None of the prognostic systems predicted overall response to HMA. Median OS for the entire cohort was 16.3 M (CI, 15.0-17.8 M). Figure 1 shows the KM survival curves and Table 1 shows the median OS, the corresponding CI and associated p-value for the risk categories in each prognostic model. Scores generated using the AIC (n=294) to assess the relative goodness of fit (lower is better) were 2139 (MDAPSS), 2148 (FPSS), 2155 (IPSS-R), and 2174 (IPSS).
Conclusions: We report the largest direct comparison of the major MDS prognostic models among HMA-treated patients. None of the models predicted overall response to HMA therapy. Nonetheless, the IPSS-R, MDAPSS, and the FPSS all functioned well to separate HMA-treated pts with HR-MDS into different prognostic groups in terms of survival. The MDAPSS and FPSS appear superior to the IPSS-R and IPSS for survival prediction. HR-MDS pts with poor projected survival with HMA therapy should be considered for up-front HCT or for experimental approaches.
| IPSS (n=595) . | IPSS-R (n=555) . | FPSS (n=296) . | MDAPSS (n=508) . | ||||
|---|---|---|---|---|---|---|---|
| Risk Group (n) | Median OS in months (CI) | Risk Group (n) | Median OS in months (CI) | Risk Group (n) | Median OS in months (CI) | Risk Group (n) | Median OS in months (CI) |
| Low (0) | NA | Very low (1) | NA | Low (19) | 38.4 (23.1-NR) | Low (4) | Not reached (NA) |
| INT-1 (0) | NA | Low (3) | 28.1 (27.0-NR) | INT (241) | 17.8 (15.9-19.6) | INT-1 (55) | 26.2 (18.8-40.4) |
| INT-2 (418) | 16.8 (15.3-18.3) | INT (59) | 39.1 (23.9-49.6) | High (36) | 10.6 (7.2-13.4) | INT-2 (143) | 18.6 (17.4-24.1) |
| High (177) | 15.2 (13.4-17.8) | High (197) | 18.8 (16.8-22.2) | High (306) | 13.4 (11.8-15.0) | ||
| Very High (295) | 12.2 (11.0-14.1) | ||||||
| P-value | P=0.014 | P<0.0001 | P<0.0001 | P<0.0001 | |||
| IPSS (n=595) . | IPSS-R (n=555) . | FPSS (n=296) . | MDAPSS (n=508) . | ||||
|---|---|---|---|---|---|---|---|
| Risk Group (n) | Median OS in months (CI) | Risk Group (n) | Median OS in months (CI) | Risk Group (n) | Median OS in months (CI) | Risk Group (n) | Median OS in months (CI) |
| Low (0) | NA | Very low (1) | NA | Low (19) | 38.4 (23.1-NR) | Low (4) | Not reached (NA) |
| INT-1 (0) | NA | Low (3) | 28.1 (27.0-NR) | INT (241) | 17.8 (15.9-19.6) | INT-1 (55) | 26.2 (18.8-40.4) |
| INT-2 (418) | 16.8 (15.3-18.3) | INT (59) | 39.1 (23.9-49.6) | High (36) | 10.6 (7.2-13.4) | INT-2 (143) | 18.6 (17.4-24.1) |
| High (177) | 15.2 (13.4-17.8) | High (197) | 18.8 (16.8-22.2) | High (306) | 13.4 (11.8-15.0) | ||
| Very High (295) | 12.2 (11.0-14.1) | ||||||
| P-value | P=0.014 | P<0.0001 | P<0.0001 | P<0.0001 | |||
Sekeres:Celgene: Membership on an entity's Board of Directors or advisory committees; Amgen Corp: Membership on an entity's Board of Directors or advisory committees; Boehringer-Ingelheim Corp: Membership on an entity's Board of Directors or advisory committees. Garcia-Manero:Novartis Pharma: Research Funding. Steensma:Amgen: Consultancy; Ariad: Equity Ownership; Celgene: Consultancy; Novartis: Consultancy. List:Celgene Corporation: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal