Abstract
Introduction: With the development of novel therapeutic agents, more than 30% of patients with multiple myeloma (MM) achieve complete response (CR) as defined by the International Myeloma Working Group (IMWG). However, most patients that achieve CR ultimately die due to relapse, suggesting the presence of minimal residual disease (MRD) in these patients. Multicolor flow cytometry (MFC) allows the detection of < 10-4 clonal plasma cells in normal bone marrow cells and has been used for detecting MRD after treatment. MFC-defined immunophenotypic response (IR) has emerged as a more relevant prognostic factor in patients with MM. However, the relevance of the prognostic impact of IR and the normalization of serum free light chain (sFLC) ratio remain unclear. We retrospectively analyzed the impact of IR, conventional immunofixation negative CR (CR), and CR plus FLC kappa/lambda (k/l) normal CR (sCR) on the prognosis of 83 patients with MM who obtained better than very good partial response (VGPR) at Kameda Medical Center, Kamogawa, Japan.
Methods: Among the 164 patients treated at our hospital between April 2005 and July 2014, 83 patients that achieved more than VGPR were included in this study. The study population consisted of 49 males and 34 females with a median age of 71 years. All patients received at least one course of novel agent-containing therapeutic regimen. Autologous stem cell transplantation was performed 43 patients. Maintenance treatment was not systematically given, but patients failed to achieve CR continued to receive treatment until CR was obtained. Treatment responses were assessed using the IMWG criteria, and the best response to treatment during the course of disease was assessed by simultaneous analysis by serum immunofixation, sFLC measurements, and MFC analysis of bone marrow plasma cells. Identification of plasma cells MFC requires at least two markers (CD38 and either CD45 or CD138) by single-tube 6-color flow-cytometry. Neoplastic plasma cells were further identified from normal plasma cell based on differential expression of CD19 and CD45 characteristics. Patients were considered MRD negative (IR) when ≤ 50 neoplastic plasma cells were detected by MFC in the bone marrow samples at the sensitivity limit of 10-4. Overall survival (OS) and Time to next treatment (TNT) differences between curves were calculated by two-sided log-rank test. Subjects were classified into three categories, i.e., CR with MRD positive or negative and VGPR, and TNT and OS were compared between groups.
Results: At a median follow-up of 44.8 months, 83 patients obtained better than VGPR, ie; CR, 55 patients, VGPR, 28 patients. Among the 55 patients who obtained CR, normalization of sFLC k/l and IR were achieved in 48 (88%) and 28 (51%) patients, respectively. Conversely, normal sFLC k/l ratio was achieved in 66 patients, 50 were in CR and 16 were in VGPR. IR was obtained in 34/83 (41%) patients. Among 48 CR patients with normal sFLC k/l (stringent CR), IR was obtained 27 patients (56%). All of the 7 CR patients with abnormal sFLC k/l (non-stringent CR) did not achieve IR.
Kaplan–Meier estimated 3- and 5-year OS were 94% and 80% in patients with CR, 90% and 71% in patients with VGPR. No significant differences were observed at 3- and 5-year OS between patients achieved CR and VGPR.
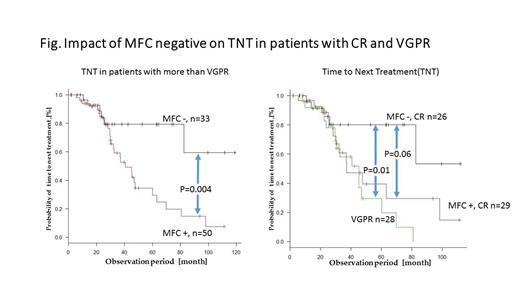
Among the patients with VGPR or better response, patients with IR showed significantly longer TNT compared to those without IR. However, The patients who achieved CR and IR showed significantly longer TNT compared to those with VGPR (P=0.004), but CR patients without IR showed similar TNT curve with VGPR patients. Patients with both CR and IR showed longer TNT than those CR but without IR, although difference between the 2 groups was marginally significant (P=0.06). Although, patients with IR and normal sFLC showed significantly longer TNT compared to those with VGPR, it was not translated to longer OS reflecting the continuous maintenance treatment for VGPR patients.
Conclusion: Although both achievement of CR, normalization of sFLC k/l, and IR appeared to confer on longer TNT and OS, obtaining IR seems to have greater implications for longer survival compared to CR or FLC k/l normalization. MFC analysis is a rapid, affordable, and easy performable method for measurement of MRD, and IR could be considered as a goal of treatment for patients with MM.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal