Abstract
Background: Patients (pts) with non-Hodgkins lymphoma (NHL) are at increased risk of venous thromboembolism (VTE). We and others have demonstrated increased risk of death among NHL pts with incident VTE; however, these studies were largely conducted in the pre-rituximab era. We therefore analyzed a large cohort of NHL pts in the California Cancer Registry (CCR), determined the incidence of VTE, and evaluated its effect on survival in the rituximab era.
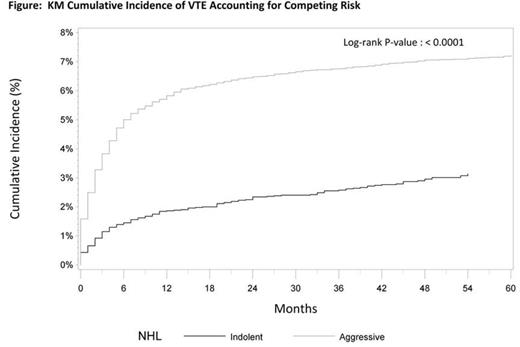
Methods: Using the CCR linked with hospital discharge and emergency department records, we identified adult NHL pts diagnosed in 2005 – 2010, excluding cases ascertained via autopsy or death certificate, and those diagnosed with acute VTE in the 2 months preceding NHL diagnosis. VTE was defined by specific ICD-9-CM codes, and Elixhauser comorbidity score, excluding lymphoma, was calculated. Cumulative incidence was calculated using the Kaplan-Meier (KM) method. Adjusted hazard ratios (aHR) of VTE and death were estimated using Cox proportional hazard models, stratified by indolent vs aggressive NHL subtype, adjusting for age, race, stage, treatment, comorbidity and prior VTE. Analyses of VTE incidence treated death as a competing risk. Cox models for death incorporated VTE as a time-dependent covariate to account for immortal time bias.
Results: NHL was identified in 18,424 pts. Most (n=12,963) had aggressive NHL (1,017 mantle cell, 11,246 diffuse large B-cell or follicular grade 3, 170 lymphoblastic, 530 Burkitt), while 5,461 had indolent NHL (2,809 follicular grade 1/2, 2,652 marginal zone). Median age was 64 years (yrs) and was similar in aggressive and indolent cohorts. Men accounted for 54% (n=9926) of cases, and were more common in aggressive compared to indolent NHL (7,317 (56%) vs 2,609 (48%) respectively). Most cases (62% n=11,451) were non-Hispanic White, 4% (n=795) were African American, 21% (n=3866) Hispanic, 11% Asian (n=2013) and 1.6% unknown (n=299). The ethnic distribution was similar in aggressive and indolent NHL. Median number of reported comorbid conditions was 2. Chemotherapy was initiated in 76% (n=9791) of aggressive NHL pts and 41% (n=2250) of indolent pts.
The KM cumulative incidence of first time, acute VTE in NHL pts was 4.7% (95% CI 4.4 – 5.0) and 5.3% (95% CI 4.9- 5.6) at 1 and 2 years respectively. The incidence of VTE was higher in patients with aggressive versus indolent NHL (6.5% (95% CI 6.1 - 6.9) vs 2.3% (95% CI 2.0 - 2.8) at 2 yrs respectively P<0.001), and was highest during the first 6 months after dx (Figure). In multivariable analysis of aggressive lymphoma pts, the risk of VTE was higher among pts receiving chemotherapy (Ctx) [aHR 2.3, 95% CI (1.9 – 3.0)], lower in pts with stage II NHL [aHR 0.8, 95% CI (0.6 – 1.0)] while histological subtype of aggressive NHL was not a predictor. For indolent NHL, the risk of developing acute VTE was increased among cases that received Ctx [aHR 2.3, 95% CI (1.6 – 3.4)], and cases with follicular grade 1/2 [aHR 1.6, 95% CI (1.1 – 2.3)] whereas stage was not a significant risk factor. Five year overall survival for aggressive NHL was 55% (95% CI 46 – 56) and 80% (95% CI 69 – 82) for indolent NHL. In multivariable analysis risk of incident VTE after diagnosis of NHL dx was associated with an increased risk of death (Table). Interestingly, this effect was present for only the first 2 years after dx of aggressive NHL, while the effect persisted throughout follow-up for indolent NHL.
Conclusions: This large, population based study, which captured essentially all patients diagnosed with NHL in California between 2005-2010, confirms prior reports of VTE incidence in NHL patients. Pts are at highest risk early in their course, and pts undergoing chemotherapy were at increased risk. Moreover, VTE subsequent to NHL diagnosis independently increases the risk of death adjusting for other important covariates. Whereas chemoimmunotherapy has negated the effect of some previous negative prognostic factors, the adverse effect of incident VTE persists in this recent cohort.
Association of VTE and Death*
| . | Aggressive NHL . | Indolent NHL . | ||
|---|---|---|---|---|
| Time from NHL dx to VTE | aHR | 95% CI | aHR | 95% CI |
| 0 – 6 months | 1.41 | 1.3 – 1.6 | 2.07 | 1.4 – 3.0 |
| 6 – 12 months | 1.40 | 1.1 – 1.8 | 2.59 | 1.4 – 4.7 |
| 12 – 24 months | 1.63 | 1.3 – 2.1 | 3.20 | 1.9 – 5.4 |
| >24 months | 0.94 | 0.7 – 1.2 | 2.37 | 1.6 – 3.6 |
| *Cox models adjusted for Age, Sex, Race, Stage, Treatment, Prior VTE and Comorbidity | ||||
| . | Aggressive NHL . | Indolent NHL . | ||
|---|---|---|---|---|
| Time from NHL dx to VTE | aHR | 95% CI | aHR | 95% CI |
| 0 – 6 months | 1.41 | 1.3 – 1.6 | 2.07 | 1.4 – 3.0 |
| 6 – 12 months | 1.40 | 1.1 – 1.8 | 2.59 | 1.4 – 4.7 |
| 12 – 24 months | 1.63 | 1.3 – 2.1 | 3.20 | 1.9 – 5.4 |
| >24 months | 0.94 | 0.7 – 1.2 | 2.37 | 1.6 – 3.6 |
| *Cox models adjusted for Age, Sex, Race, Stage, Treatment, Prior VTE and Comorbidity | ||||
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal