Abstract

INTRODUCTION
Nephrotic Syndrome, one of the most common forms of glomerular disease, is characterized by massive proteinuria with structural and functional injury of specialized glomerular cells called podocytes. There is evidence to indicate that thrombin generation is enhanced in nephrotic syndrome. The massive protein loss in nephrotic syndrome includes loss of key coagulation regulators, leading to a complex coagulopathy, enhanced thrombin activating capacity and, consequently, increased risk for devastating thromboembolic complications. Recent in vitro studies have demonstrated that exposure to high concentrations of thrombin can injure podocytes, suggesting that thrombin may exacerbate glomerular injury. However, the molecular mechanisms by which thrombin induces podocyte injury are not yet known. Thrombin activates platelets, leukocytes, and other cells via the protease activated receptor (PAR) system. Thus, we hypothesized that thrombin exacerbates glomerular injury by enhancing podocyte apoptosis in a PAR-dependent manner.
METHODS
Experiments were performed with differentiated, conditionally immortalized human and rat podocytes. After 36 hours of thrombin (20nM) exposure podocyte apoptosis was determined by TUNEL assay. In human podocytes, specific PAR antibodies and activating peptides were utilized to determine which PARs mediate thrombin-induced podocyte apoptosis. Specific PAR antibodies (ab) included hPAR1ab (ATAP2), hPAR2 ab (SAM11), hPAR3 ab (8E8), hPAR4 ab (H-120). Activation peptides (AP) included PAR1 AP (TFFLRNPNDKNH2), PAR2 AP (SLIGRLNH2); PAR3 AP (TFRGAPOH); PAR4 AP (AYPGKFNH2) and a control peptide (FSLLRNNH2). Phalloidin assays were used to evaluate structural changes in the actin-cytoskeleton as a marker of podocyte stress. We have established that human thrombin is hemostatically active and regulated in rat plasma. Thus, rat podocytes were exposed to human thrombin, to determine toxicity, and specific PAR antibodies to determine if blockade of PARs could ameliorate thrombin mediated toxicity. One-Way ANOVA and t-tests were used to determine statistical significance (SigmaPlotTM).
RESULTS
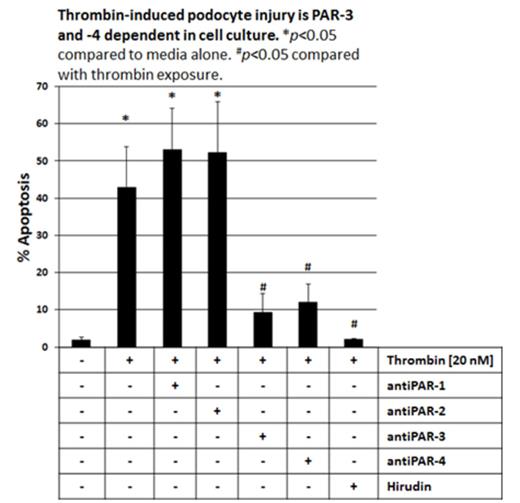
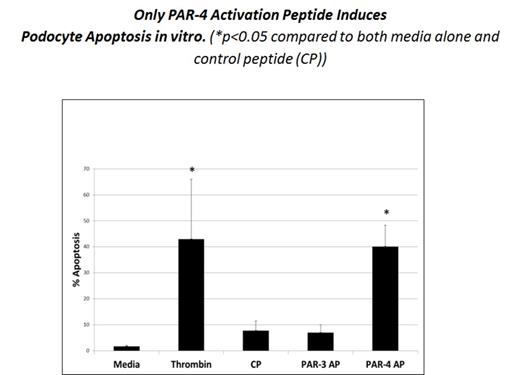
Thrombin exposure induced a significant increase in apoptosis of human podocytes from 1.8% to 42.87% (p<0.05). Blockade of PAR-3 or PAR-4 resulted in a significant decrease in apoptosis [9.2% with hPAR-3 ab and 11.7% with hPAR-4ab] (p<0.05). Inhibition of thrombin enzymatic activity with hirudin, a direct thrombin inhibitor, also resulted in a decrease in apoptosis to 2.1% (p<0.05). In comparison to a control peptide, PAR-4 activation peptide significantly increased apoptosis from 1.7% to 40.1% (p<0.05), while PAR-3 activation peptide did not. Analogous results were seen with the phalloidin assay. Thrombin caused actin cytoskeletal changes, while PAR-3 and PAR-4 blockade ameliorated these changes. In addition, only activation with PAR-4 activating peptide resulted in loss of actin stress fibers.
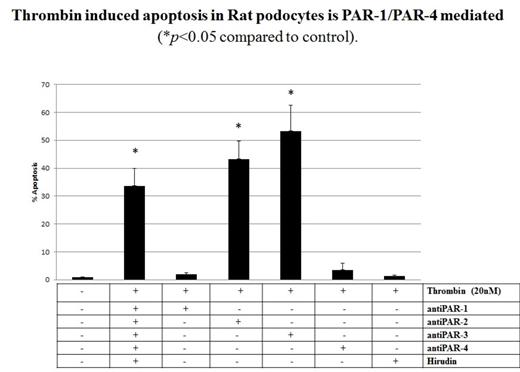
In rat podocytes human thrombin had a similar effect with increased apoptosis from 1% to 33.6% (p<0.05). We also demonstrated that this may be a PAR-mediated mechanism as blockade of PAR-1 and PAR-4 with specific antibodies ameliorated thrombin induced apoptosis [1.94% with PAR-1 ab and 3.5% with PAR-4ab] while blockade of PAR-2 and PAR-3 did not have a similar effect (p<0.05).
CONCLUSIONS
Thrombin-induced injury is mediated in a PAR-dependent fashion in both humans and rats. Specifically, in this in vitro model, thrombin induced apoptosis appears to be mediated in a PAR-3/-4 dependent manner in human podocytes but in a PAR-1/-4 manner in rat podocytes. Furthermore, these data suggest that thrombin induced podocyte injury may be mediated in a manner dependent on PAR heterodimerization. Our findings collectively suggest that interrupting thrombin-mediated podocyte injury may offer a novel future therapeutic approach to reduce podocyte injury in nephrotic syndrome.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal