Abstract
Background: Cancer patients are at high risk of developing venous thromboembolism (VTE). However, the actual risk of VTE varies widely between individual patients and therefore in the past years several studies have focused on the identification of risk factors for cancer-associated VTE. Red cell distribution width (RDW) has been reported to be associated with arterial and venous thrombosis in non-cancer patients and with mortality in several diseases. RDW is a parameter of the complete blood count that describes the size variation of red blood cells (RBC). Here, we analyzed the association between RDW and other RBC parameters with risk of VTE and mortality in patients with cancer.
Methods: RBC parameters (RDW, hematocrit, hemoglobin concentration, mean corpuscular volume, mean corpuscular hemoglobin and mean corpuscular hemoglobin concentration) were measured in 1840 patients with cancers of the lung (=309), breast (n=273), brain (n=245), colon/rectum (n=182), prostate (n=157), pancreas (n=130), stomach (=63), kidney (n=42); lymphoma (n=260), multiple myeloma (n=49) and other tumor sites (n=130) that were included in the Vienna Cancer and Thrombosis Study (CATS). CATS is an ongoing prospective, observational cohort study of patients with newly diagnosed or progressive cancer after remission. Primary study outcome is occurrence of symptomatic VTE and secondary outcome is death during a maximum follow-up period of 2 years.
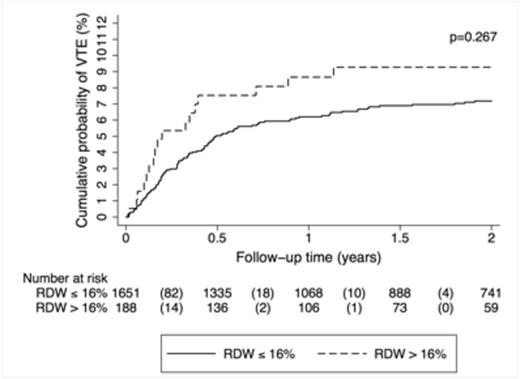
Results: During a median follow-up of 706 days, 131 (7.1%) patients developed VTE and 702 (38.2%) died. High RDW (>16%) was not associated with a higher risk of VTE in the total study cohort; in competing risk analysis accounting for death as competing variable the univariable subhazard ratio (SHR) was 1.34 (95% confidence interval [CI]: 0.80-2.23, p=0.269). In patients with high RDW (>16%), the cumulative probability of VTE was 7.5% after 6 months, 8.7% after one year and 9.3% after two years in comparison to a probability of 5.0% after 6 months, 6.2% after one year and 7.2% after two years in those patients who had a lower RDW (Gray's test p=0.267; Figure 1). There was also no significant association between other RBC parameters and risk of VTE.
In subgroup analysis of patients with solid tumors only, high RDW (>16%) was associated with an 80% increase in risk of VTE compared to lower RDW (SHR [95% CI]: 1.80 [0.99-3.26], p=0.053). However, in multivariable analyses adjusting for age, sex, hemoglobin, leukocyte and platelet count we did not observe a significant association between RDW and risk of VTE (SHR [95% CI]: 1.57 [0.81-3.04], p=0.182).
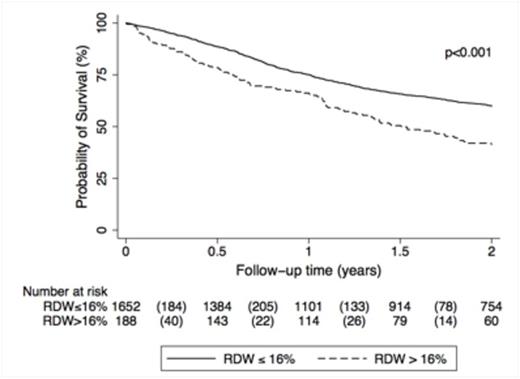
High RDW was associated with an increased risk of mortality in the total study population (hazard ratio [HR, 95% CI]: 1.72 [1.39-2.12], p<0.001), and this association prevailed after adjustment for age, sex, hemoglobin, leukocyte and platelet count (HR [95% CI]: 1.34 [1.06-1.70], p=0.016). The cumulative probability of survival in patients with high RDW (>16%) was 78.5% after 6 months, 66.2% after one year and 41.3% after two years. In comparison, patients with non-elevated RDW levels had a cumulative survival probability of 88.7% after 6 months, 75.1% after one year and 66.2% after two years (Log-rank p<0.001; Figure 2).
Conclusions: RDW and other RBC parameters were not independently associated with risk of VTE in patients with cancer and might therefore not be of added value for estimating risk of VTE in patients with cancer. We could confirm that high RDW is an independent predictor of poor overall survival in cancer.
Cumulative incidence of venous thromboembolism (VTE), accounting for competing risk (death of any cause) in the total study cohort, grouped into patients with red cell distribution width (RDW) >16% and below, respectively.
Cumulative incidence of venous thromboembolism (VTE), accounting for competing risk (death of any cause) in the total study cohort, grouped into patients with red cell distribution width (RDW) >16% and below, respectively.
Kaplan-Meier estimates for cumulative survival probability of cancer patients (total study cohort) with red blood cell distribution width (RDW) >16% and below, respectively.
Kaplan-Meier estimates for cumulative survival probability of cancer patients (total study cohort) with red blood cell distribution width (RDW) >16% and below, respectively.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal