Abstract
On Behalf of the European MCL Pathology Panel
Introduction: Mantle-cell lymphoma (MCL) is an aggressive B-cell lymphoma with a median overall survival (OS) of 5 years, but clinical course varies considerably. This variability has been partly explained by clinical characteristics forming the MIPI (Hoster et al., JCO 2014), but also biological and histological features such as tumor cell proliferation (Ki-67 index), cytology, or growth pattern (Tiemann et al., BJH 2005). Immuno-chemotherapy induction represents the current standard of care, in younger patients including high-dose cytarabine and followed by autologous stem cell transplantation, whereas older patients benefit from rituximab maintenance (Dreyling et al., Ann Oncol 2013). In 2004, the European MCL Network started two large randomized trials, MCL Younger and MCL Elderly, for previously untreated MCL patients. Histopathological features of diagnostic samples were centrally assessed by the European MCL Pathology Panel. Since MCL is relatively rare, evaluations of prognostic factors were mostly based on smaller, retrospectively collected patient cohorts. We now aimed to comparatively evaluate the prognostic value of Ki-67 index, cytology, and growth pattern using the data of these trials.
Methods: The Ki-67 index was counted according to published guidelines (Klapper et al., J Hematopathol 2009). MCL cytology was classified as classic, small-cell (B-CLL-like), pleomorphic (DLBCL-like), or blastic (LB-like) (Vogt and Klapper, Histopathology 2013). MCLs with pleomorphic or blastic cytology were combined to blastoid MCL. The growth pattern was classified as diffuse (≤50% nodular) or non-diffuse (>50% nodular or predominantly mantle-zone pattern). The prognostic relevance of these markers was evaluated with respect to OS, adjusting for MIPI score.
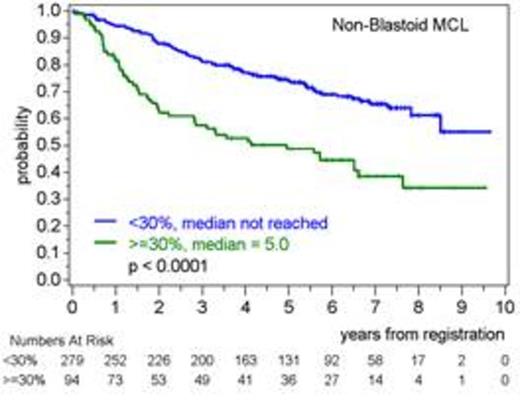
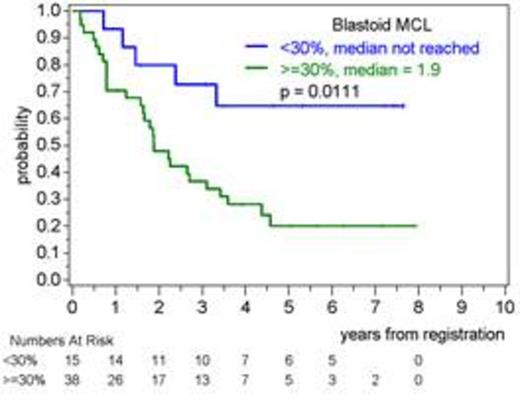
Results: Of 1012 trial patients with MCL, Ki-67 index, cytology, or growth pattern were available in 50%, 61%, and 47%, respectively. Reasons for missing information were mainly insufficient material or staining. Median Ki-67 index was 20% (2%-97%). 88% had classic MCL, 2% small-cell, 7% pleomorphic and 3% blastic cytology, summing up to 10% with blastoid MCL. 63% of patients had a diffuse growth pattern. Higher Ki-67 index, blastoid MCL, and diffuse growth were each associated with higher MIPI score. Growth pattern was not clearly associated with Ki-67 index or cytology, whereas pleomorphic (median Ki-67 index 39%, range 7%-90%) or blastic MCL (median 80%, 29%-97%) displayed a substantially higher Ki-67 index compared non-blastoid MCL (median 19%, 2%-95%). In univariable analyses, the adjusted OS hazard ratios for higher Ki-67 index (10% increase), blastoid MCL, or diffuse growth were 1.16 (95% CI 1.09-1.24, p<0.0001), 1.91 (1.34-2.72, p=0.0004), and 1.16 (0.84-1.60, p=0.38), respectively. In multivariable analyses, Ki-67 index was more relevant (adjusted hazard ratio 1.12, 1.04-1.22, p=0.0032) than blastoid MCL (1.46, 0.94-2.29, p=0.095), whereas growth pattern was not prognostic. Accordingly, patients with Ki-67 index ≥30% had substantially inferior OS than patients with Ki-67 index <30% in both, blastoid and non-blastoid MCL (Figure 1).
Conclusions: In a large cohort of MCL patients treated in randomized trials according to current guidelines, tumor cell proliferation (Ki-67 index) was a powerful prognostic marker, superior to cytology and growth pattern, and independent of clinical prognostic factors. The Ki-67 index further stratified patients with non-blastoid as well as patients with blastoid MCL into groups with substantially different survival. Thus, standardized assessment of the Ki-67 index (Klapper et al. J Hematopathol 2009) should be routinely performed in clinical practice to allow a more comprehensive individual risk estimation of MCL patients. Further analyses will aim at the biological basis of this prognostic effect.
Overall survival according to Ki-67 index (< vs. ≥ 30% from Determann et al., Blood 2008) in patients with non-blastoid (left) or blastoid (right) mantle-cell lymphoma (MCL)
Overall survival according to Ki-67 index (< vs. ≥ 30% from Determann et al., Blood 2008) in patients with non-blastoid (left) or blastoid (right) mantle-cell lymphoma (MCL)
Dreyling:Roche: Honoraria, Research Funding. Klapper:Roche: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal