Abstract
Background: Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma (NHL) in our institution (49.5%). The World Health Organization (WHO) classification recognizes several subtypes of DLBCL based on morphology, immunohistochemistry (IHC) and molecular analysis. A half of patients remain incurable with standard strategy with anti-CD20 monoclonal antibody (rituximab) and anthracycline-based chemotherapy. Therefore, it is necessary to identify high risk patients to try to improve their prognosis. In the pre-rituximab era, the best way to identify this high-risk group was based on International Prognostic Index (IPI) and more recently on molecular aspects that characterizesthe gene signature of the malignant cell. Patients with gene expression profile similarto normal cells from germinal center (GC) showed better prognosis than those with B-cells activated signature. Correspondentsalgorithms based in IHC were also proposed and that proposed by Hans is the most commonly used.However, these prognostic indicators have been questioned in the rituximab era. On the other hand, currently,the positron emission tomography with 18 F-fluodeoxyglucose (PET 18 F-FDG) has been recommended at diagnosis and at the endof treatment to improve accuracy of staging and response evaluation. Even though some studies have shown improvement on survival in patients with negative PET after 2-3 cycles of R-CHOP it impact as a prognostic factor in DLBCL remains controversial.
Objective: This study was proposed to investigate the association between interim PET (iPET) and cellular origin of DLBCL using Hans' algorithm as prognosis in patients treated with R-CHOP.
Methods: Were analyzed prospectively 146 DLBCL patients treated with R-CHOP 21.The 18 F-FDG PET was performed after 2 cycles of R-CHOP and at the end of treatment in 105 patients. DLBCL was classified asGC and NGC subtype by IHC using Hans's algorithm .
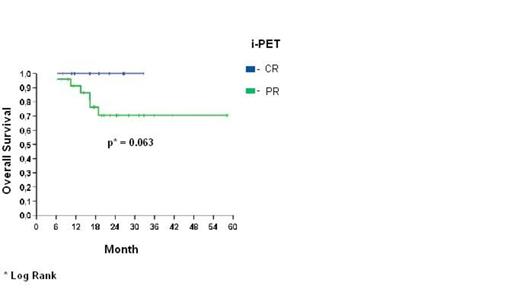
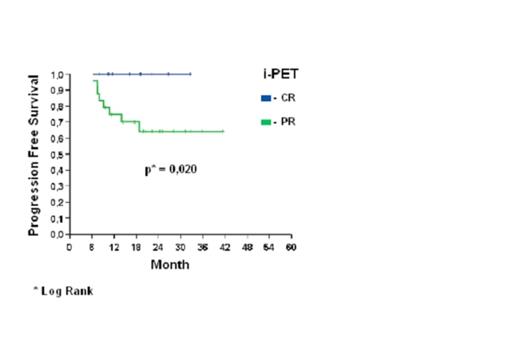
Results: The median age of GC-DLBCL (52.7 years) was lower than NGC-DLBCL (59.4 years) (p=0.021) and in patients with negative iPET (52.7 years) versus positive iPET (59.4 years) (p=0.031). Bulky disease was more common in GC-DLBCL (p=0.008). The overall survival (OS) at 30 months for GC-DLBCL was 100% for patients with negative iPET and 70,4% for patients with positive iPET (p=0.063) (Figure 1). Progression-free survival (PFS) at 30 months was 100% for GC-DLBCL and iPET negative and 64,3% for GC-DLBCLand iPET positive (p=0.02) (Figure 2).
Conclusion: We concluded that iPET and cell origin determination by Hans's immunohistochemical algorithm was able to identify a subgroup of very good prognosis showing GC origin and negative iPET. However, our results should be confirmed in others studies.
Analysis of overall survival in patients with GC-DLBCL according to positivity of iPET.
Analysis of overall survival in patients with GC-DLBCL according to positivity of iPET.
Analysis of progression-free survival in patients with GC-DLBCL according to positivity of iPET.
Analysis of progression-free survival in patients with GC-DLBCL according to positivity of iPET.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal