Abstract
Background
Chronic lymphocytic leukemia (CLL) is the most common leukemia in western country. Although the prognosis is improved in the last years, CLL is still an incurable disease and infections are the major cause of morbidity and mortality. Susceptibility to infections in CLL patients can be an intrinsic characteristic of the disease or due to chemo-immunotherapy. Immunoglobulin (Ig) replacement therapy is a safe and effective way to prevent infectious events in CLL patients, but indications to their use are not strictly defined.
The aim of this study was to determine risk factors to serious bacterial infections in CLL patients and to identify a clinical phenotype of patients characterized by a high infectious risk, in which Ig replacement therapy (IgRT) is appropriate.
Methods
We retrospectively analyzed clinical and biochemical data of 706 patients, referred to the Hematology and Clinical Immunology Unit of Padua University Hospital since 1982. In this series, we identify patients with at least one episode of major infections (MI), defined as pneumonia, sepsis, meningitis, and endocarditis. We considered only non neutropenic MI.
FISH analyses (n=450), CD38 expression (n=529), ZAP70 (n=502), IGHV (n=473), TP53, NOTCH1, BIRC3, SF3B1 (176 genes tested) mutational status, were evaluated before at diagnosis or before starting treatment. Staging and Ig levels were collected at the time of the MI; for patients who didnÕt complain any MI we recorded the last available data. Inferior normal values for IgG, IgA and IgM were 7.0, 0.70 and 0.40g/dL, respectively.
Continuous variables were compared by Mann-Whiney test, while categorical variables by Fisher exact test or Chi-square test, when appropriated. Overall survival (OS) was calculated from the date of initial presentation to death for any cause (event) or last known follow-up (censored). Survival analyses were performed by Kaplan-Meier method. Log-rank test was used to compare overall survival curves between groups and Cox regression models to estimate hazard ratios. The proportional hazard assumption was tested in all cox models. p values <0.05 were considered significant and <0.0005 as highly significant. 95% confidential intervals (CI), positive predictive value (PPV) and negative predictive valure (NPV) were also reported.
Results
69 patients (9.8%) had 89 MI, among these 62 were pneumonia (3 pulmonary aspergillosis), 21 sepsis, 1 meningitides, 1 cerebral abscess, 1 uveitis and 1 endocarditis.
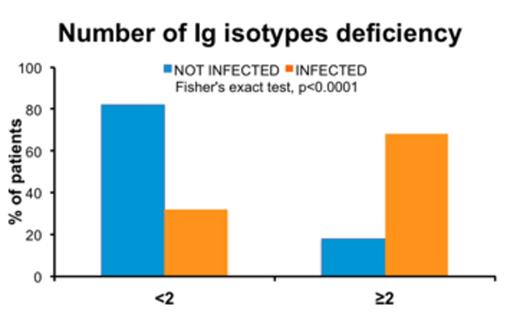
We observed a higher risk of MI in subject with at least 2 Ig isotypes deficiencies (Figure 1, Odds Ratio 10.1 (CI 5.78-17.6), p<0.0001); PPV and NPV were 29% and 96%, respectively. By contrast, patients with only 1 Ig deficiency did not show a higher risk of MI.
Clinical-biological characteristics between patients with MI (PwI) and without MI (PwoI) were skewed, in particular the formers harbored a high-risk cytogenetic (i.e. del17p and del11q, p<0.0001), unmutated IGHV (homology>98%, p=0.0043), CD38+ (>30%, p=0.0205), were at a more advance stage (Rai III-IV, p<0.0001) and experienced treatment (p<0.0001). No differences were found neither for ZAP70 expression (>20%, p=0.6775), nor TP53, NOTCH1, BIRC3, SF3B1 gene mutations (p=0.9998), nor chemotherapy regiments (p=0.1587).
Considering PwI and at least 2 Ig isotypes deficiencies (n=47), 21 patients treated with IgRT showed a reduction of the incidence of MI (0.70 MI/patient/year in the 12 months before IgRT and 0.27 MI/patient/year during replacement therapy).
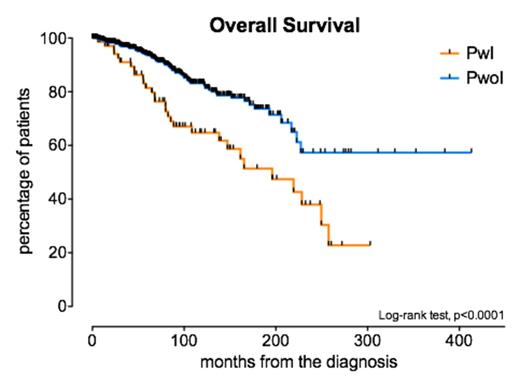
Kaplan-Meier analysis showed that PwI had a shorter OS than PwoI with a median OS of 196 months vs not reached, respectively (Figure 2, p<0.0001). 10-years OS were 64.7% and 83.4% for PwI and PwoI, respectively. In multivariate analysis highly significant variables were history of MI, del17p and U-IGHV. In particular PwI had 2.3 (CI 1.5-3.6, p<0.0001) higher risk of death than PwoI patients.
Discussion
In our work, we described the prognostic role of MI in CLL patients, superimposable to other main prognostic factors. Moreover, we identified the clinical profile of patients at high risk of major infections: low levels of at least 2 Ig isotypes, aggressive disease (U-IGHV, del17p) and previous treatment. We also described the reduction of the incidence of MI in a small cohort of 21 patients after IgRT. Taking advantage from this study, we will investigate safety and usefulness of Ig prophylaxis in a bigger subset of patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal