Abstract
Background: Re-admission to the hospital within 30 days is a measure for quality care and a point of emphasis for reducing health care costs in individuals with chronic disease. Potentially modifiable risk factors for 30 day re-admission in children with sickle cell disease (SCD) includes not being seen in the SCD clinic within 30-days of discharge (OR 7.7, 95% CI 2.4–24.4), 3 or more admissions in the previous 12 months (OR 7.3, 95% CI 2.8–18.9) and co-morbid asthma (OR 2.9, 95% CI 1.2–7.3) (Pediatr Blood Cancer. 2009 Apr;52(4):481-5). Limited data exists regarding potentially modifiable risk factors for 30-day re-admission in adults with SCD. The primary objective of this study was to define modifiable risk factors for 30-day re-admission in adults with SCD, leading to a prospective intervention study to decrease re-admission rates.
Procedure: At a tertiary care center, we performed a retrospective analysis of the medical records, from 2010 to 2013, to determine risk factors for 30-day re-admission in adults with SCD. Initial admission was defined as the first admission associated with uncomplicated vaso-occlusive pain episode in each focus year (2011- 2013). To decrease bias associated with multiple admissions from the same individual, the first admission for vaso-occlusive pain in each year was evaluated as the index admission for each record. Cases and controls were defined as adults with SCD initially admitted for pain and subsequently re-admitted to the hospital within 30 days of the initial admission. A multi-variable logistic regression analysis was performed on seven postulated risk factors. All data was collected and double checked by a single reviewer, and at least 10% of the chart was checked by a medical student for further assurance of accuracy.
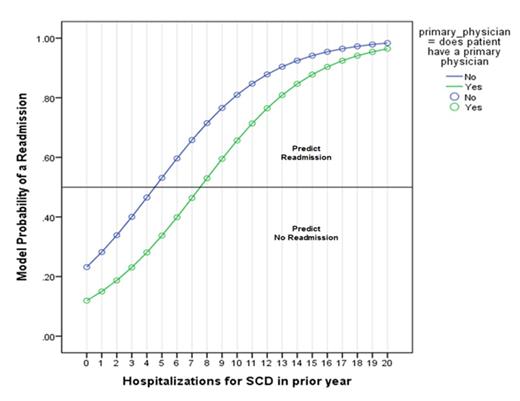
Results: A total of 158 first admissions and 49 re-admissions (31%) were evaluated. The mean age of the cohort was 30.38 (IQR 13.55 years). The median time to re-admission was 10 days (IQR 19 days). Approximately 50% of the cohort was not evaluated in the outpatient setting by the hematology team within 30 days post-discharge. Upon discharge patients either were not given a follow up appointment (35%) or were given an appointment beyond 30 days of discharge (13%). Only two predictors were significantly associated with re-admission within 30 days: not having a primary care provider listed in the electronic medical record (odds ratio 0.35, 95% CI 0.146-0.858; p = 0.022) and the number of hospital admissions due to vaso-occlusive pain in the prior year (odds ratio 1.28, 95% confidence interval 1.15-1.42; p < 0.001), table and figure below. Five covariates were not significantly associated with re-admission within 30 days: age (odds ratio 0.982, 95% CI 0.94-1.02; p = 0.369), sex (odds ratio 0.715, 95% CI 0.28-1.81, p =0.481), hemoglobin phenotype (odds ratio 0.50, 95% CI 0.19-1.287; p = 0.15), median lifetime oxygen saturation (odds ratio 0.892, 95% CI 0.75-1.05; p = .186), and presence of government insurance (odds ratio 1.90, 95% CI 0.67-5.37; p =0.222).
Conclusions: Not having a primary care provider listed in the electronic medical record and multiple admissions in the prior year are potentially modifiable risk factors for re-admission within 30 days in adults with SCD. In addition, discharge planning with a hematology visit scheduled within a week of discharge may also impact the 30-day re-admission rate. We recently introduced a strategy focused on improved discharge planning, ensuring a primary care provider for every adult patient with SCD and targeted therapeutic intervention for those with high admissions.
Multivariable analysis of risk factors for 30-day re-admission in adults with sickle cell disease over a course of 3 years. A total of 158 admissions were evaluated with 31% being re-admissions within 30 days.
| . | Sig. . | Odds ratio . | 95% C.I.for EXP(B) . | |
|---|---|---|---|---|
| Lower . | Upper . | |||
| Age Upon Admission to the Hospital | 0.369 | 0.982 | 0.944 | 1.021 |
| Sex | 0.481 | 0.715 | 0.281 | 1.817 |
| Hemoglobin Phenotype | 0.152 | 0.504 | 0.197 | 1.287 |
| Median Lifetime Oxygen Saturation Level | 0.186 | 0.892 | 0.753 | 1.057 |
| Primary Care Provider | 0.022 | 0.354 | 0.146 | 0.858 |
| Government Insurance | 0.222 | 1.907 | 0.676 | 5.378 |
| Number of Hospitalizations Due to Vaso-Occlusive Pain in the Prior Year | 0.000 | 1.278 | 1.148 | 1.422 |
| . | Sig. . | Odds ratio . | 95% C.I.for EXP(B) . | |
|---|---|---|---|---|
| Lower . | Upper . | |||
| Age Upon Admission to the Hospital | 0.369 | 0.982 | 0.944 | 1.021 |
| Sex | 0.481 | 0.715 | 0.281 | 1.817 |
| Hemoglobin Phenotype | 0.152 | 0.504 | 0.197 | 1.287 |
| Median Lifetime Oxygen Saturation Level | 0.186 | 0.892 | 0.753 | 1.057 |
| Primary Care Provider | 0.022 | 0.354 | 0.146 | 0.858 |
| Government Insurance | 0.222 | 1.907 | 0.676 | 5.378 |
| Number of Hospitalizations Due to Vaso-Occlusive Pain in the Prior Year | 0.000 | 1.278 | 1.148 | 1.422 |
A graph depicting the predicted probablity of a re-admission within 30 days in indivdiuals with and without hospitalization versus the number of hospitalizations in the prior years.
A graph depicting the predicted probablity of a re-admission within 30 days in indivdiuals with and without hospitalization versus the number of hospitalizations in the prior years.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal