Abstract
Introduction: Venous thromboembolism (VTE), defined as deep vein thrombosis (DVT), pulmonary embolism (PE), or both, is an important cause of morbidity and mortality among hospitalized patients, with PE ranking among the most frequent undiagnosed acute diseases in medical practice (Adv Orthop,2010;2(1):8–14).
Methods: Durham County, NC, has a population of ~280,000 individuals and is served by three hospitals, Duke University Medical Center (DUMC) and Duke Regional Hospital (DRH) that share an electronic medical record, and the Durham Veterans’ Administration Medical Center (VAMC). Autopsy service is performed primarily at DUMC and, much less frequently, at the Durham VAMC. We performed a retrospective review of all autopsies performed at DUMC during a two year period (April 1st 2012 through March 31st 2014). Individuals living outside of Durham County were excluded. We also excluded autopsies performed on fetuses and neonates less than one month of age, as well as autopsies that were limited to examination of the brain only. Autopsies at DUMC are generally limited to the chest, abdomen and pelvis, and the limbs are typically not examined. VTE identified at autopsy, therefore, included PE and DVT involving the inferior vena cava and the abdominal, iliac, brachiocephalic, subclavian, and/or internal jugular veins. For Durham county patients with autopsy-proven VTE, we reviewed the medical records for the clinical characteristics of these individuals, including whether VTE was clinically suspected (or known) prior to death. To evaluate the total number of deaths in Durham county residents within the same time period, we obtained data from the Durham county Register of Deeds office and the NC Vital Records office.
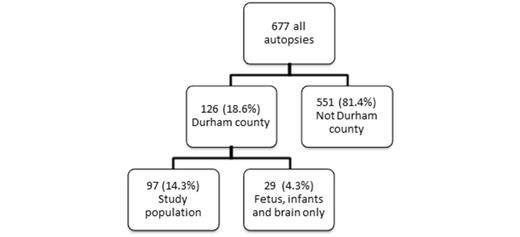
Results: During the two year study period, a total of 677 autopsies were performed at DUMC as shown in the figure below.
Of the 97 autopsies on patients from Durham county, VTE was diagnosed at autopsy in 19 cases (19.6%). The mean age of patients diagnosed with VTE at autopsy was 54 years (range 21-82 years). Ten were male (53%). Characteristics of the events are summarized in the table below.
| Type of event . | Hospitalization at the time of death. . | Thromboprophylaxis prior to death. . | VTE diagnosed antemortem . |
|---|---|---|---|
| Subsegmental PE only (n=6) Segmental PE only (n=2) Both (n=4) | 5 2 3 | 3 2 2 | 1 0 0 |
| DVT* (n=6) | 5 | 3 | 1 |
| PE and DVT* (n=1) | 1 | 0 | 0 |
| Total (n=19) | 16 | 10 | 2 |
| Type of event . | Hospitalization at the time of death. . | Thromboprophylaxis prior to death. . | VTE diagnosed antemortem . |
|---|---|---|---|
| Subsegmental PE only (n=6) Segmental PE only (n=2) Both (n=4) | 5 2 3 | 3 2 2 | 1 0 0 |
| DVT* (n=6) | 5 | 3 | 1 |
| PE and DVT* (n=1) | 1 | 0 | 0 |
| Total (n=19) | 16 | 10 | 2 |
* DVT involved the following veins: hepatic vein (2), left common iliac (1), internal jugular vein (1), inferior vena cava (1), “central” venous (1), and the mesenteric and pelvic veins (1)
Slightly more than half the patients who were hospitalized at the time of death were receiving some type of thromboprophylaxis, and two of the patients had been diagnosed with VTE prior to their death.
According to the pathologist’s report, PE was the direct cause of death in 4 cases. All patients had one or more risk factors for VTE as shown in table below.
| Predisposing Factor . | Occurrence, n (%) . |
|---|---|
| Hospitalization | 16 (84%) |
| Age >40 | 12 (63%) |
| Surgery | 6 (32%) |
| Obesity | 6 (32%) |
| Cancer | 6 (32%) |
| Diabetes mellitus | 5 (26%) |
| Central venous catheter | 3 (16%) |
| Prior known VTE | 1 (5%) |
| Predisposing Factor . | Occurrence, n (%) . |
|---|---|
| Hospitalization | 16 (84%) |
| Age >40 | 12 (63%) |
| Surgery | 6 (32%) |
| Obesity | 6 (32%) |
| Cancer | 6 (32%) |
| Diabetes mellitus | 5 (26%) |
| Central venous catheter | 3 (16%) |
| Prior known VTE | 1 (5%) |
One of the limitations of this analysis is the small number of autopsies that are currently performed in the US. During the two year period, a total of 3918 residents of Durham county died within the state of NC. The rate of autopsy for Durham County residents who died during the study period, therefore, was only 2.5% of all deaths during this period.
Conclusions: The frequency of VTE identified at autopsy in our retrospective study is 19.6% (19 of 97). The majority of these patients were not suspected to have VTE prior to death. Although most were hospitalized, more than a third were not receiving thromboprophylaxis at the time of death. Hospitalization is a common risk factor for VTE, and VTE remains an important cause of death in hospitalized patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal