Abstract

On-going public health surveillance efforts in sickle cell disease (SCD) are critical for understanding the course and outcomes of this disease over time. Once nearly universally fatal by adolescence, many patients are living well into adulthood and sometimes into retirement years. Previous SCD mortality estimates have relied on data from death certificates alone or from deaths of patients receiving care in high volume hematology clinics, resulting in gaps in reporting and potentially biased conclusions.
The Registry and Surveillance System for Hemoglobinopathies (RuSH) project collected and linked population-based surveillance data on SCD in California and Georgia from a variety of sources for years 2004-2008. These data sources included administrative records, newborn screening reports and health insurance claims as well as case reports of adult and pediatric patients receiving care in the following large specialty treatment centers: Georgia Comprehensive Sickle Cell Center, Georgia Regents University, Georgia Comprehensive Sickle Cell Center at Grady Health Systems and Children's Healthcare of Atlanta in Georgia, and Children's Hospital Los Angeles and UCSF Benioff Children's Hospital Oakland in California. Cases identified from these combined data sources were linked to death certificates in CA and GA for the same years.
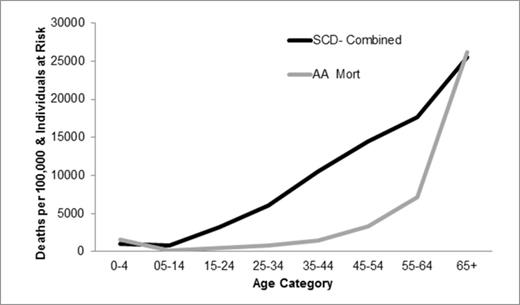
Among 12,143 identified SCD cases, 640 were linked to death certificates. Combined SCD mortality rates by age group at time of death are compared to combined mortality rates for all African Americans living in CA and GA. (Figure 1). SCD death rates among children up to age 14 and among adults 65 and older were very similar to those of the overall African American population. In contrast, death rates from young adulthood to midlife were substantially higher in the SCD population.
Overall, only 55% of death certificates linked to the SCD cases had SCD listed in any of the cause of death fields. Thirty-four percent (CA) and 37% (GA) had SCD as the underlying cause of death. An additional 22% and 20% (CA and GA, respectively) had underlying causes of death that were not unexpected for SCD patients, including related infections such as septicemia, pulmonary/cardiac causes of death, renal failure and stroke. The remaining 44% (CA) and 43% (GA) had underlying causes of death that were either not related to SCD (e.g., malignancies, trauma) or too vague to be associated with SCD (e.g., generalized pulmonary or cardiac causes of death. Figure 2 shows the number of deaths by state, age group at death and whether the underlying cause of death was SCD specific, potentially related to SCD or not clearly related to SCD. While the number of deaths was too small to use for life expectancy calculations, there were more deaths over age 40 than under age 40 during this five year period.
This effort represents a novel, population-based approach to examine mortality in SCD patients. These data suggest that the use of death certificates alone to identify deceased cases may not capture all-cause mortality among all SCD patients. Additional years of surveillance are needed to provide better estimates of current life expectancy and the ability to track and monitor changes in mortality over time. On-going surveillance of the SCD population is required to monitor changes in mortality and other outcomes in response to changes in treatments, standards of care and healthcare policy and inform advocacy efforts.
This work was supported by the US Centers for Disease Control and Prevention and the National Heart, Lung and Blood Institute, cooperative agreement numbers U50DD000568 and U50DD001008.
SCD-Specific & Overall African American Mortality Rates in CA and GA, 2004 – 2008.
SCD-Specific & Overall African American Mortality Rates in CA and GA, 2004 – 2008.
Deaths (Count) Among Individuals with SCD in CA and GA, by Age Group and Underlying Cause of Death, 2004-2008 (N=615)
Deaths (Count) Among Individuals with SCD in CA and GA, by Age Group and Underlying Cause of Death, 2004-2008 (N=615)
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal