Abstract
Introduction
Diagnosis and classification of acute myeloid leukemia (AML) are based on morphology and genetics. FMS-like tyrosine kinase 3 internal tandem duplication (FLT3-ITD), FMS-like tyrosine kinase 3 tyrosine kinase domain (FLT3-TKD) and nucleophosmin1 gene (NPM1) are most frequent mutations found in patients with AML. In this study, we aimed to identify the prognostic value of FLT3 and NPM1 mutations in our AML patients.
Method
We retrospectively evaluated 121 patients who had been diagnosed based on the WHO AML diagnosis criteria, between 2007 and 2014 in the Department of Hematology at Ankara University. FLT3 and NMP 1 mutations were detected by Polymerase chain reaction (PCR) amplification method. The overall survival (OS) and relapse-free survival (RFS) due to FLT3 and NMP1 mutations were analyzed using Kaplan Meier method and Long-Rank. P<.05 was considered statistically significant.
Results
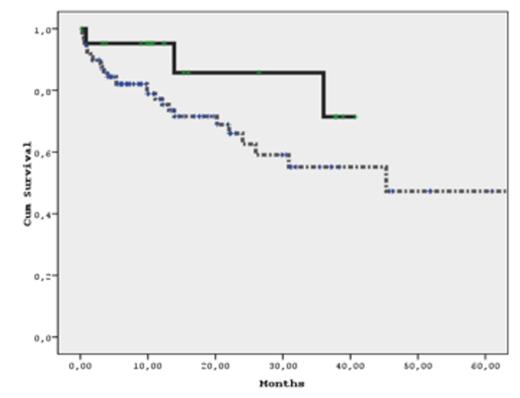
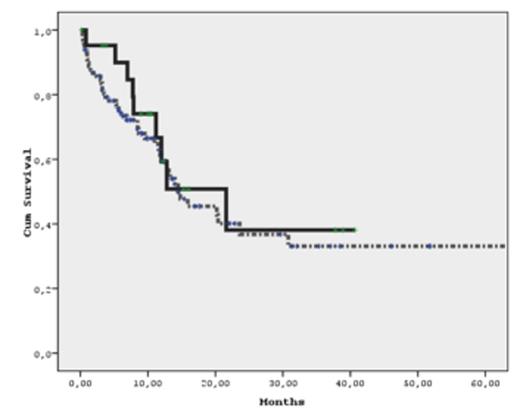
Of the 121 patients, 50 (41%) were female and 71 were male (59%). The mean diagnosis age of AML in the female patients was 50.52 ± 2.23, whereas the mean diagnosis age in the male patients was 50.62 ± 2.15. 115 of 121 patients (95%) received cytarabine (ARA-C) and an anthracycline ("7+3" protocol) as an remission induction therapy while 6 of the patients (5%) haven't received any therapy because of older age and poor performance status. 33 of 121 patients (33%) got cytarabine (ARA-C) and an anthracycline ("7+3" protocol) as a reinduction therapy. 67 of 121 patients (55%) were followed by consolidation therapy with high-dose ARA-C. Allogeneic stem cell transplantation (ASCT) was performed in 31 of 121 patients (31%) during follow-up. The donors were relatives in 21 of 31 patients (68%) while 10 ASCT were from unrelated donors (32%). 32 of 121 patients (26%) were dead during follow-up. The FLT3 and NMP1 mutations were studied from peripheral blood in 27 of 121 patients (22%) while in 94 of 121 (78%) patients samples from bone marrow were used. 27 of 121 patients (22%) had NMP1 mutation positive whereas 22 of 121 patients (18%) had FLT3 mutation positive. In 4 of 22 patients were FLT3-TKD positive others were FLT3-ITD positive.The FLT3 positive patients are significantly older than FLT3 negative patients (P<.05) Due to flow cytometric analysis, 17 of 121 patients (14%) were considered as low risk. 3 of 17 low risk patients had FLT3 mutation positive (18%) and 2 of them were diagnosed as AML M3 (12%). The median OS in FLT3 mutation positive group was 17.93 ± 13.86 months, whereas the median OS was 15.03±14.90 months in FLT3 mutation negative group. In NMP mutation positive patients the median OS was 14.53±13.03 months while in NMP mutation negative groups the median OS was 15.85±15.20 months. The median RFS in FLT3 mutation positive group was 13.38±11.59 months, whereas the median RFS was 11.98±12.79 months in FLT3 mutation negative group. In NMP mutation positive patients the median RFS was 12.26±12.11 months while in NMP mutation negative groups the median RFS was 12.23±12.73 months. In subgroup analysis, the median OS in FLT3-ITD mutation positive group was 15.34±13.03 months while 14.29±14.65 months of median OS was detected in FLT3-ITD negative patients. On the other hand, the median RFS was 10.10±9.32 months in FLT3-ITD positive patients and 11.46±12.40 months in FLT3-ITD negative patients. Neither FLT3 mutation (FLT3-ITD or both FLT3-ITD and FLT3-TKD) nor NMP mutation positive patients are statistically different from FLT3 or NMP mutation negative patients due to OS and RFS (P>.05)(Figure 1)(Figure 2).
Conclusion
In previous studies, FLT3-ITD mutation predicted an unfavorable prognosis whereas mutation in NPM1 gene was associated with favorable prognosis. Unexpectedly we detected no difference in either OS or RFS in FLT3 or NPM1 gene mutated patients.
Kaplan Meier Curve of OS in FLT3 positive and negative group(dashed curve FLT3 positive).
Kaplan Meier Curve of OS in FLT3 positive and negative group(dashed curve FLT3 positive).
Kaplan Meier Curve of RFS in FLT3 positive and negative group (dashed curve FLT3 positive).
Kaplan Meier Curve of RFS in FLT3 positive and negative group (dashed curve FLT3 positive).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal