Abstract
BACKGROUND: The programmed cell death-1 ligands (PD-Ls; PD-L1 and PD-L2) act as negative regulators of anti-tumor immunity by binding their cognate receptor, PD-1, on cytotoxic T-cells and inducing T-cell "exhaustion", a phenotype that is reversible with PD-1 blockade. Human antibodies that block PD-1 induce objective clinical responses in the majority of patients with relapsed / refractory classical Hodgkin Lymphoma (CHL).
CHLs include small numbers of malignant Hodgkin Reed-Sternberg (HRS) cells (~5% of total cellularity) within an extensive but ineffective inflammatory and immune cell infiltrate. Over 85% of CHLs express PD-Ls on both the HRS cells and additional non-malignant cells within the tumor microenvironment (Chen et al., CCR 2010). PD-L expression in HRS cells is attributable, in part, to copy gain of chromosome 9p24.1, a region that includes PD-L1, PD-L2, and JAK2 (Green et al., Blood, 2010). However, the contribution of non-malignant cells to the overall PD-L expression within the tumor micro-environment of CHL is poorly defined.
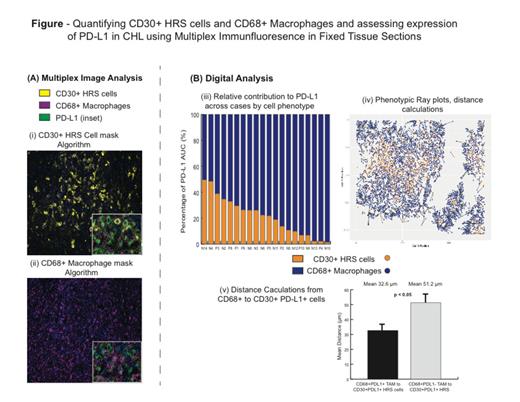
METHODS: We analyzed select CHLs (12 EBV+, 8 EBV-) by multiplex immunofluorescence using formalin-fixed, paraffin embedded tissue sections, with successive labeling by primary antibodies (PD-L1, CD30, CD68, pSTAT3, CD163), followed by secondary amplification and tyramide-conjugated fluorophores. For each case 2 large representative areas of tissue, totaling eight 20x fields of view were selected and imaged using a multispectral imaging platform. Two specific image analysis algorithms were designed to accurately identify CD30+ HRS cells and CD68+ macrophages simultaneously, then to threshold PD-L1 by relative fluorescent units (RFU) in each phenotype. Cartesian coordinates for all cells were exported and distance calculations were generated between PD-L1+ and PD-L1- macrophages and their Ônearest neighborÕ CD30+ PD-L1+ HRS cell.
RESULTS: The percentages of CD30+ HRS cells and CD68+ macrophages expressing PD-L1 was highly variable across cases (range 9 - 94%, median 46.6% for HRS cells; range 6 - 91.3%, median 48.2% for macrophages). In all cases the majority of PD-L1 protein within the tumor micro-environment was contributed by macrophages (median 77.9%, range 50.4 - 98.5%), although the mean relative intensity of PD-L1 per cell was higher for HRS cells than for macrophages (3.13 +/-0.02 RFU vs 2.85 +/- 0.01 RFU; p < 0.0001 by Welch t-test). Further analysis revealed that the percentage of HRS cells and macrophages expressing PD-L1 was highly correlated (Pearson r = 0.67; 95% CI 0.32 - 0.85; p=0.001) and, in 18/20 tumors, PD-L1+ macrophages were in greater proximity to PD-L1+ HRS cells than PD-L1- macrophages (across 20 cases mean distance of 32.6 µm (SE 5 µm) versus 51.2 µm (SE 6.8 µm), respectively; p < 0.05).
CONCLUSIONS: CD68+ tumor-associated macrophages (TAMs) express the majority of PD-L1 in CHLs, which contain rare tumor cells. Image analysis of the distribution of PD-L1 in the tumor microenvironment indicates that PD-L1+ TAMs are significantly enriched in proximity to PD-L1+ HRS cells. These data implicate HRS cells in coordinating PD-L1 induction among TAMs to limit anti-tumor immunity.
Shipp:Merck: Membership on an entity's Board of Directors or advisory committees; Gilead: Consultancy; BMS: Membership on an entity's Board of Directors or advisory committees, Research Funding; Sanofi: Research Funding; Bayer: Membership on an entity's Board of Directors or advisory committees, Research Funding. Rodig:Perkin Elmer: Membership on an entity's Board of Directors or advisory committees; Bristol Myers Squibb: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal