Abstract
BACKGROUND: Non-Hodgkin B cell lymphomas are often infiltrated by immune effector cells including T, NK and dendritic cells. But despite their presence within the tumor they fail to control tumor growth. Some T cells can even play a supportive role to maintain the tumor and prevent the function of anti-tumor immune cells.
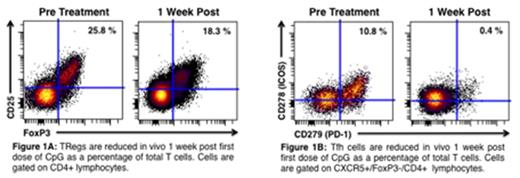
Regulatory T cells (TRegs) function normally to dampen immune responses and prevent auto-immunity by direct cell contact or by secreting suppressive cytokines i.e. TGF-b and Interleukin-10. Follicular Lymphoma tumor cells can induce the conversion of CD4 T cells into TRegs (1-3), thereby evading anti-tumor immune responses.
Follicular helper T cells (Tfh), another class of regulatory T cells, are found within normal follicles of lymphoid organs. Migrating into the germinal center, they promote the survival and differentiation of follicular B cells. In lymphoma, Tfh cells can send a survival signal to tumor B cells through CD40L/CD40 interactions (4).
STUDY: In an ongoing multi-center phase I clinical trial (NCT02266147), patients with previously untreated low-grade lymphoma receive low dose (2Gyx2) radiotherapy to a single, tumor site, followed by intratumoral injection into the same site of a CpG-ODN (SD-101, Dynavax Technologies), an immune-modulatory molecule that targets Toll-like Receptor 9 (TLR-9). Doses ranged from 1mg to 8mg per injection in successive cohorts. A fine needle aspirate (FNA) of the treated site is performed before, one week after the first injection, and 1 week after the 5th and final weekly injection of CpG-ODN. FNA samples are sent to a central site by overnight delivery in media with 5% fetal calf serum. They are processed within 24 hours and stained for flow cytometry with panels of antibodies to delineate T, B, NK, dendritic, myeloid cells, and their subsets. Antibodies against activation antigens, as well as T cell exhaustion, inhibition and function are also used to characterize these cells.
To date, 12 patients have been entered into the dose escalation phase of this study: 10 follicular lymphoma, 1 chronic lymphocytic lymphoma and 1 small lymphocytic lymphoma. Nine of 12 patients had FNAs that yielded enough viable cells for evaluation pre and 1 week post treatment.
RESULTS: Therapy has been well tolerated. Local injection site reactions and fever, the most common side effects, resolved by 48 hours. There have been no related SAEs. The treated site regressed in all patients per CT scan at 3 months post treatment. The early evaluation of untreated lesions documented 1 PR. The remaining patients have stable disease with all but one having systemic tumor regressions ranging from 14% to 28%.
Seven out of 9 patients evaluable by flow cytometry had an increase in total T cells at the treated site 1 week following the first dose of CpG ranging from 18 to > 300% above baseline in both the CD4 and CD8 compartments. More interestingly, there was a reduction of TRegs as a percentage of total T cells in 7 of 9 patients (average reduction: 21.3 ± 10.6%). A single patient with an increase in untreated tumor burden of 15% showed no reduction in TRegs. There was also a reduction of Tfh cells in 8 of the 9 evaluable patients (average reduction: 87.2 ±7.2%). One patient with SLL had no Tfh cells pretreatment. Figure 1A and B shows a representative example of TReg and Tfh cell depletion within the same FL patient.
CONCLUSION: Immune modulating therapies can be delivered directly into a tumor to minimize systemic toxicity and induce changes in the tumor microenvironment while potentially inducing a global anti-tumor immune response. In this case, the combination of intratumoral CpG and low-dose radiation reduced the proportion of TRegs and Tfh cells, thereby modulating their immune inhibitory effects and tumor growth promoting effects, respectively. This clinical trial is ongoing and open to accrual.
Monitoring the cell populations in the tumor site by repetitive sampling and analysis by flow cytometry reveals the pharmocodynamic effects of anti-cancer therapies, especially those intended to trigger anti-tumor immune responses. This knowledge can be used to tailor therapies and to influence the choice and scheduling of combinations of agents designed to target specific cell populations.
1. Yang Z-Z, et al. Blood. 2007;110:537-44.
2. Ai WZ, et al. Int J Cancer. 2009 Jan 1;124(1):239-44.
3. Mittal S, et al. Blood. 2008;111:5359-70.
4. AmŽ-Thomas P, et al. Blood. 2015 Apr 9;125(15):2381-5
Bartlett:Gilead: Consultancy, Research Funding; Janssen: Research Funding; Pharmacyclics: Research Funding; Genentech: Research Funding; Pfizer: Research Funding; Novartis: Research Funding; Millennium: Research Funding; Colgene: Research Funding; Medimmune: Research Funding; Kite: Research Funding; Insight: Research Funding; Seattle Genetics: Consultancy, Research Funding; MERC: Research Funding; Dynavax: Research Funding; Idera: Research Funding; Portola: Research Funding; Bristol Meyers Squibb: Research Funding; Infinity: Research Funding; LAM Theapeutics: Research Funding. Gordon:Northwestern University: Employment; Dr Leo I. Gordon: Patents & Royalties: Patent for gold nanoparticles pending. Coffman:Dynavax Technologies: Employment. Janssen:Dynavax Technologies: Employment. Levy:Bullet Biotechnology, Inc.: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal