Abstract

Portal hypertension is a common complication of myeloproliferative neoplasms (MPN) and portends a poor prognosis. Arising in 7-18% of MPN patients, portal hypertension develops through several distinct mechanisms, including abdominal vein thrombosis, extramedullary hematopoiesis (EMH), and nodular regenerative hyperplasia (NRH). Similar to cirrhotic patients, MPN-associated portal hypertension presents with refractory ascites, gastrointestinal bleeding, hepatic encephalopathy, and susceptibility to infections. Transjugular intrahepatic portosystemic shunt (TIPS) procedure has been used empirically to treat refractory ascites and variceal bleeding in MPN-related portal hypertension; however, there is limited data in regards to TIPS effectiveness in MPN-associated portal hypertension. To assess the safety and efficacy of TIPS for treatment of portal hypertension in MPN, we performed a retrospective analysis of outcomes of TIPS procedure in patients with MPN in our institution.
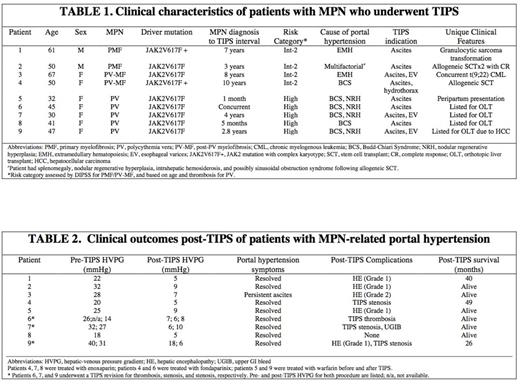
Using the University of Pennsylvania electronic medical record database, we identified nine patients with MPN who underwent TIPS procedure for treatment of refractory portal hypertension between 2005 and 2015. Patients with portal hypertension from causes other than MPN were excluded from the study. Clinical characteristics and long-term outcomes were analyzed.
The mean age at time of TIPS was 47 years (range 30-67 years). Seven of nine patients were female (78%) and all seven carried a diagnosis of polycythemia vera (PV) or post-PV myelofibrosis (PV-MF); both male patients had a diagnosis of primary myelofibrosis (PMF) (Table 1). All nine patients were positive for JAK2V617F mutation, and one patient had a concurrent diagnosis of Philadelphia-chromosome positive CML. The most common etiology of portal hypertension was Budd-Chiari Syndrome (BCS) in six patients (67%), followed by NRH in five patients (56%), and EMH in two patients (22%); one patient had several distinct causes of MPN-related portal hypertension. Indications for TIPS included refractory ascites in five patients (63%), ascites and esophageal varices in three patients (33%), and ascites and hydrothorax in one patient. All patients demonstrated immediate normalization of portal pressures following TIPS without any reported periprocedural complications (Table 2). Additionally, all patients received indefinite anticoagulation (low molecular weight heparin, 3 patients; vitamin K antagonist, 2 patients; fondaparinux, 2 patients). TIPS intervention had 1-year patency rate of 89%. However, one third of patients required subsequent shunt revision at a median interval of 22.3 months (range 10-34 months) due to stent stenosis or thrombosis despite anticoagulation; one patient had radiographic evidence of TIPS dysfunction without clinical symptoms. Of note, all three patients who developed TIPS stenosis/thrombosis had BCS and NRH. The majority of patients (89%) experienced complete resolution of ascites, while the remaining patient had partial improvement in ascites but no longer required routine paracentesis. Grade 1 and 2 hepatic encephalopathy was the most common complication post-TIPS (67%), occurring in half of the patients with BCS and in all three patients with portal hypertension due to EMH. One patient had variceal bleeding in the setting of TIPS thrombosis. All patients were alive 2 years post-TIPS (excluding one patient with recent TIPS; range 2-5 years).
Our study represents the first systematic analysis of outcomes of TIPS procedure for management of portal hypertension in MPN using data from a single-institution over a ten-year period. Our results suggest that TIPS procedure can be performed safely in this high-risk population, and can effectively mitigate the clinical consequences of portal hypertension in patients with MPN. However, the prevalence of TIPS complications, particularly of TIPS stenosis/thrombosis and hepatic encephalopathy, remains significant and must be balanced against the desired clinical benefits. Future studies with a larger number of patients are needed to delineate prognostic factors that identify MPN patients most likely to benefit from TIPS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal