Abstract
Introduction
It is acknowledged that an accurate histological diagnosis may distinguish Essential Thrombocythemia (ET) from early Primary Myelofibrosis (early-PMF), which is projected to worse outcome in terms of survival and disease evolution into acute leukemia (AL) or overt myelofibrosis (MF). It is also accepted that the outcome of ET is related to the mutational status, with JAK2V617F mutation having a negative impact. In previous analyses, outcome data derived from the admixture of the two variables, histology and mutational status. Here, we present a large cohort of ET/early-PMF patients positive for the JAK2V617F mutation, with the aim to evaluate the impact on outcome of the sole histological definition.
Methods
A clinic-pathologic database of ET patients followed in four Italian Hematology Centers was created and a total of 475 WHO-diagnosed ET or early-PMF JAK2V617F-positive patients was collected. Bone marrow specimens were performed or reviewed at local institution. Baseline clinical/molecular characteristics and outcome measures (vascular complications, disease transformation/progression, overall and event-free survival) were evaluated. In all patients, JAK2V617F allele-burden was assessed in granulocyte DNA by using ipsogen JAK2 MutaQuant Kit (qPCR). The study was approved by the Ethic Committee of each participating Centers.
Results
Overall, 329 WHO-defined ET and 146 early-PMF patients positive for the JAK2V617F mutation were included in the study. Median follow-up was 6.6 years (range: 0.5-32.4). Compared to ET patients, early-PMF patients presented with older age (median, 57 versus 53.5yr, p=0.02), lower hemoglobin levels (median, 14.2 versus 14.5 g/dl, p=0.01), higher leukocyte count (median, 10.4 versus 9.5x109/l, p=0.01), and higher incidence of spleen enlargement (35.9% versus 13.9%, p<0.001). JAK2V617F mutation was heterozygous in 90% and 87% of ET and early-PMF patients, respectively (p=0.34). Use of antiplatelet and cytoreductive therapies was also comparable in the two groups. During follow-up, 32 (9.7%) ET and 18 (12.3%) early-PMF patients experienced a total of 59 thrombotic events (arterial: 49%), with an incidence rate of 1,3% patients/yr. The cumulative incidence of thrombosis was 8% and 14% at 5 and 10 years, respectively. Overall, 27 patients (5,6%) and 6 (1.2%) patients evolved to MF and AL, respectively. The cumulative incidence of disease progression into MF/AL was 2% and 5% at 5 and 10 years, respectively. At last contact, 28 (5.8%) patients had died, at a median age of 77.5 years (20-88), for an overall survival of 93.8% at 10 years. In early-PMF compared to ET, the 10-year survival rates (91.6% and 95%, respectively, p=0.75), leukemic transformation rates (6% and 1.2%, respectively, p=0.45) and rates of thrombosis (6.7% and 2.2%, p=0.12) were comparable. However, progression to overt MF at 5 years (4.4% and 0.9%, respectively) and 10 years (11.5% and 1.5%) was significantly worse (p=0.004). Multivariable analysis confirmed this finding and also identified homozygosity for the JAK2V617F mutation (p=0.008) as additional risk factor for disease evolution into secondary MF.
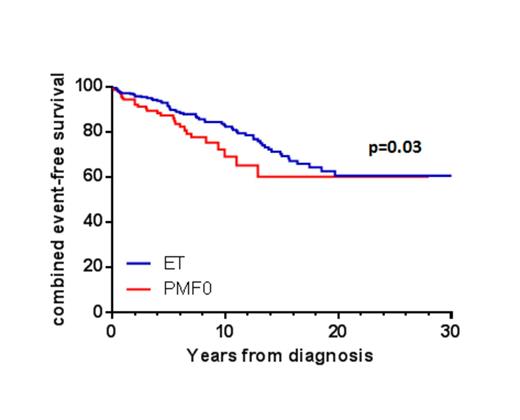
The rate of composite outcomes (thrombosis, evolution into overt MF or AL and death) was significantly higher in early-PMF (3.1% vs 2,3% pts/yr) with a combined event-free survival of 69% versus 82% in ET patients at 10 yrs (figure 1).
Conclusions. This study eliminates the confounding factor of different molecular status on outcome by focusing on a large cohort of WHO-defined ET/early-PMF patients, all carrying the JAK2V617F mutation. Overall, the study validates the clinical relevance of strict adherence to WHO criteria on prognosis, and particularly on disease progression into secondary MF.
Palumbo:Novartis: Honoraria, Other: Advisory Board. Martinelli:MSD: Consultancy; BMS: Speakers Bureau; Roche: Consultancy; ARIAD: Consultancy; Novartis: Speakers Bureau; Pfizer: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal